Monday Poster Session
Category: Liver
P2985 - Portal Hypertension-Associated Gastric Polyp: A Source of Upper Gastrointestinal Bleeding in Cirrhosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Sunny Sandhu, MD
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Rama Tarakji, MD1, Sunny Sandhu, MD2, Elizabeth Montgomery, MD2, Paul Martin, MD2
1Mount Sinai Medical Center, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Although esophageal varices (EV) are the most common etiology of gastrointestinal hemorrhage in cirrhosis, upper gastrointestinal bleeding may occur from other manifestations of portal hypertension including gastric varices, portal hypertensive gastropathy (PHG), and gastric antral vascular ectasia (GAVE). Gastric polyps are a common endoscopic finding and are typically benign and incidental. However in patients with cirrhosis, polyps may develop as a consequence of portal hypertension. We present a patient with alcohol-related cirrhosis who developed symptomatic anemia necessitating hospitalization from an actively bleeding gastric PHP that was successfully managed with resection.
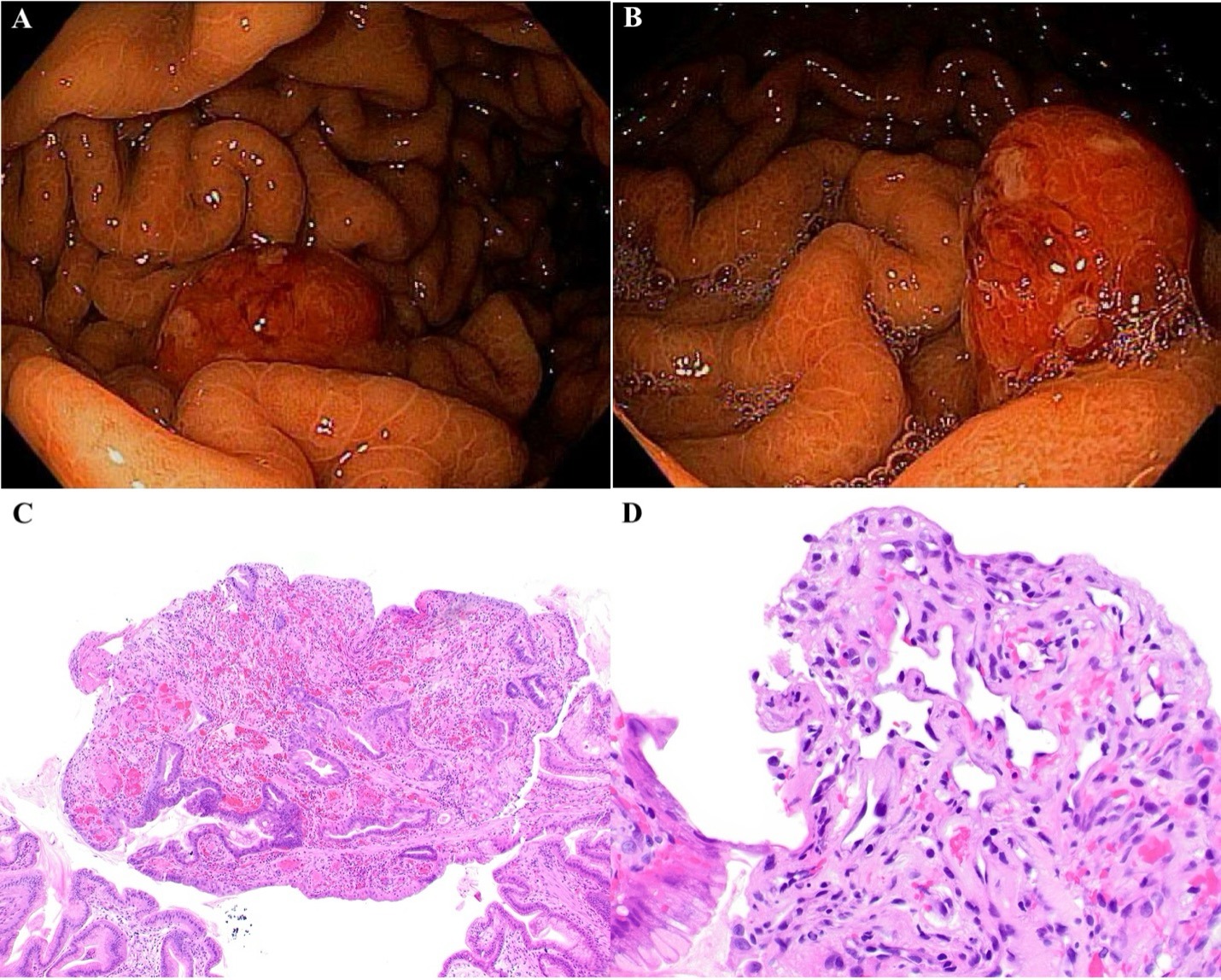
Case Description/Methods: A 63-year-old male with alcohol-associated liver cirrhosis, complicated by ascites, non-bleeding esophageal varices, and hepatic encephalopathy, presented to the emergency department with symptomatic anemia and melena. Laboratory studies showed Hb 6.9 g/dL, ALT 31 U/L, AST 20 U/L, ALP 89 U/L, total bilirubin 2 mg/dL, albumin 2.6 g/dL, INR 1.7. EGD showed large EV without high-risk stigmata, moderate PHG, and three gastric polyps, the largest measuring 12mm with an adherent clot and active oozing and was resected with hot snare (Figure 1). Pathology showed a benign PHP involving the antral and transitional mucosa (Figure 1). The patient was monitored with no signs of further bleeding, and discharged home in stable condition. At 2-month follow-up, he has had no signs of recurrent anemia.
Discussion: Portal hypertension-associated gastric polyps are uncommonly encountered, benign lesions in about 1-3% of patients with cirrhosis based on limited retrospective studies, and are typically incidentally found. Compared to hyperplastic polyps, PHPs are often larger and contain more vascular capillaries, a result of neoangiogenesis due to portal hypertension. The clinical course of PHPs is not well characterized. The vast majority do not require intervention, and significant bleeding is a rare complication. The optimal management of PHPs is not also defined, however resection as in our case was effective in controlling bleeding. In patients with portal hypertension, PHP needs to be considered as a source of non-variceal hemorrhage.
Disclosures:
Rama Tarakji, MD1, Sunny Sandhu, MD2, Elizabeth Montgomery, MD2, Paul Martin, MD2. P2985 - Portal Hypertension-Associated Gastric Polyp: A Source of Upper Gastrointestinal Bleeding in Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai Medical Center, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Although esophageal varices (EV) are the most common etiology of gastrointestinal hemorrhage in cirrhosis, upper gastrointestinal bleeding may occur from other manifestations of portal hypertension including gastric varices, portal hypertensive gastropathy (PHG), and gastric antral vascular ectasia (GAVE). Gastric polyps are a common endoscopic finding and are typically benign and incidental. However in patients with cirrhosis, polyps may develop as a consequence of portal hypertension. We present a patient with alcohol-related cirrhosis who developed symptomatic anemia necessitating hospitalization from an actively bleeding gastric PHP that was successfully managed with resection.
Case Description/Methods: A 63-year-old male with alcohol-associated liver cirrhosis, complicated by ascites, non-bleeding esophageal varices, and hepatic encephalopathy, presented to the emergency department with symptomatic anemia and melena. Laboratory studies showed Hb 6.9 g/dL, ALT 31 U/L, AST 20 U/L, ALP 89 U/L, total bilirubin 2 mg/dL, albumin 2.6 g/dL, INR 1.7. EGD showed large EV without high-risk stigmata, moderate PHG, and three gastric polyps, the largest measuring 12mm with an adherent clot and active oozing and was resected with hot snare (Figure 1). Pathology showed a benign PHP involving the antral and transitional mucosa (Figure 1). The patient was monitored with no signs of further bleeding, and discharged home in stable condition. At 2-month follow-up, he has had no signs of recurrent anemia.
Discussion: Portal hypertension-associated gastric polyps are uncommonly encountered, benign lesions in about 1-3% of patients with cirrhosis based on limited retrospective studies, and are typically incidentally found. Compared to hyperplastic polyps, PHPs are often larger and contain more vascular capillaries, a result of neoangiogenesis due to portal hypertension. The clinical course of PHPs is not well characterized. The vast majority do not require intervention, and significant bleeding is a rare complication. The optimal management of PHPs is not also defined, however resection as in our case was effective in controlling bleeding. In patients with portal hypertension, PHP needs to be considered as a source of non-variceal hemorrhage.
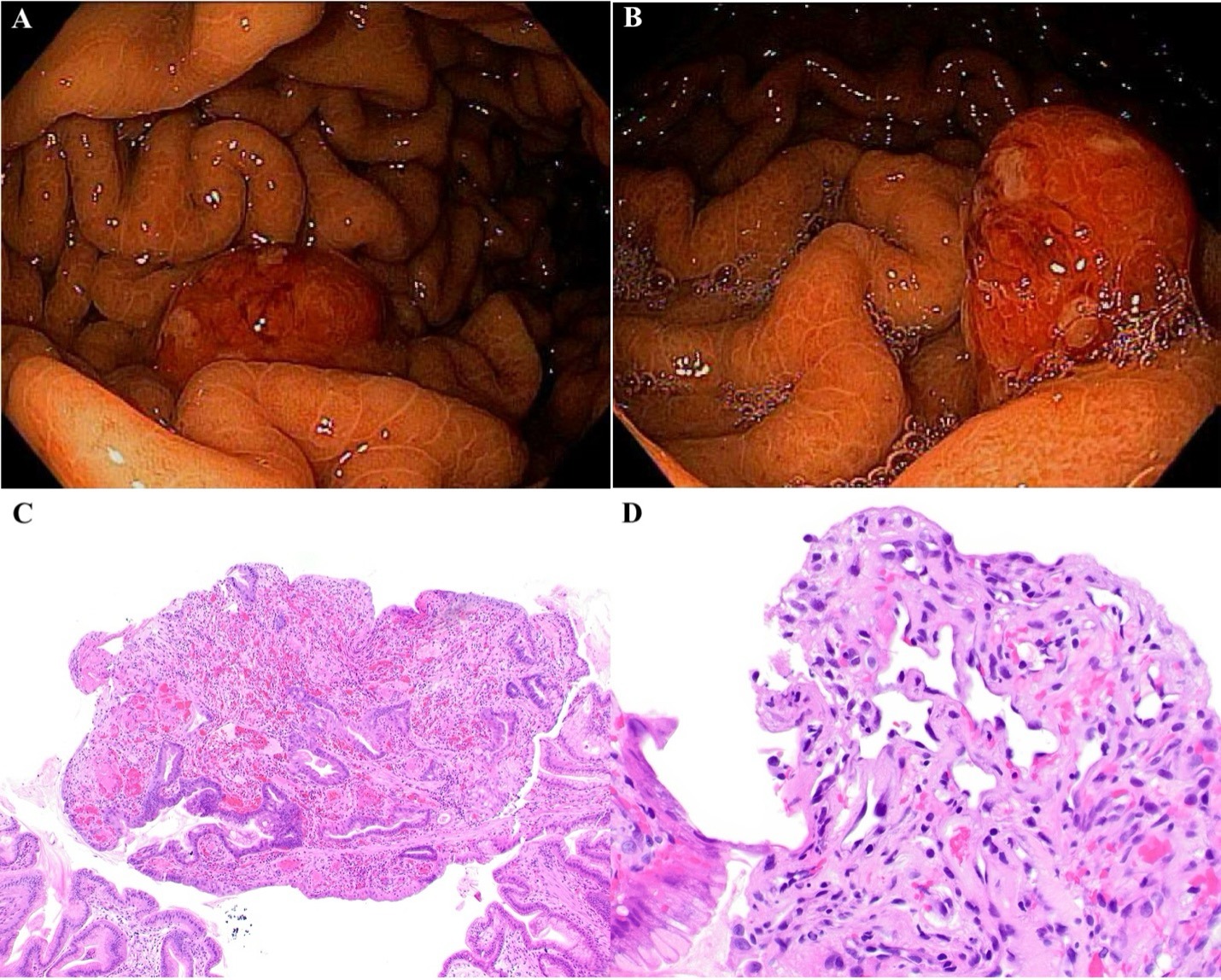
Figure: Figure 1: (A) and (B): Endoscopic view of 12mm gastric polyp with an adherent clot and active oozing. (C): Portal hypertension-associated gastric polyp. Striking vascular ectasia is present. Several fibrin thrombi are present at the left side of the image. (D): Portal hypertension-associated gastric polyp. Although the surface foveolar cells are artifactually absent in this image, capillaries just beneath the surface are dilated and lined by plump endothelial cells with a hobnail appearance.
Disclosures:
Rama Tarakji indicated no relevant financial relationships.
Sunny Sandhu indicated no relevant financial relationships.
Elizabeth Montgomery indicated no relevant financial relationships.
Paul Martin indicated no relevant financial relationships.
Rama Tarakji, MD1, Sunny Sandhu, MD2, Elizabeth Montgomery, MD2, Paul Martin, MD2. P2985 - Portal Hypertension-Associated Gastric Polyp: A Source of Upper Gastrointestinal Bleeding in Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
