Monday Poster Session
Category: Liver
P2986 - Hepatocellular Carcinoma in Cirrhosis Due to Cystic Fibrosis Liver Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SS
Sunny Sandhu, MD
University of Miami Miller School of Medicine
Miami, FL
Presenting Author(s)
Rama Tarakji, MD1, Sunny Sandhu, MD2, Paul Martin, MD2
1Mount Sinai Medical Center, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Cystic fibrosis liver disease (CFLD) has been well-described in the pediatric population, however with increased life expectancy rates, a second wave has been observed in recent years in adults, and currently represents the third most common cause of death. Although complications from portal hypertension have been described in the setting of CFLD, the development of hepatocellular carcinoma (HCC) is an extremely rare event which has only described in 3 other cases. We present a patient with CFLD who developed HCC that was successfully treated with microwave ablation.
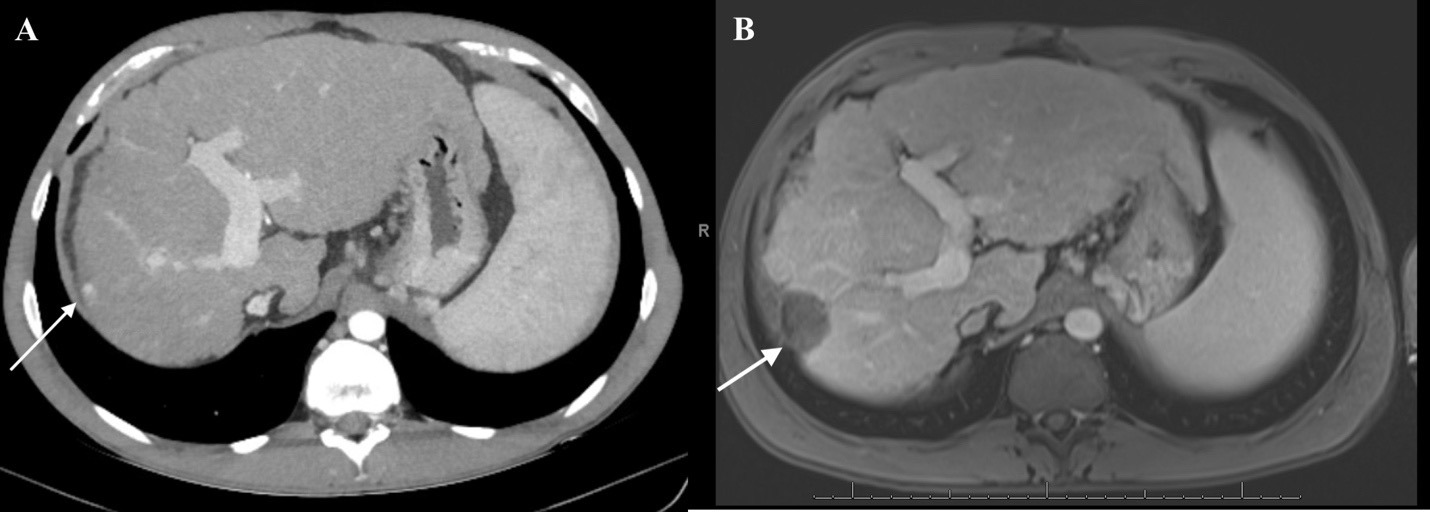
Case Description/Methods: A 36-year-old male with CF diagnosed at age 6, complicated by pancreatic exocrine insufficiency, pulmonary manifestations, and 10-year history of cirrhosis with ascites and non-bleeding esophageal varices, was under routine surveillance of CFLD. Laboratory studies showed ALT 19 U/L, AST 29 U/L, ALP 77 U/L, total bilirubin 0.6 mg/dL, albumin 3.7 g/dL, INR 1.1, alpha-fetoprotein (AFP) 1.4 ng/mL. CT triple-phase showed a new LI-RADS 3, 1cm arterial hyper-enhancing nodule in segment 7. Close interval imaging 3 months later showed a LI-RADS 4 lesion with interval growth to 1.2cm with arterial enhancement and washout on delayed imaging (Figure 1). Given the short-interval growth and concerning imaging findings in the setting of long-standing cirrhosis, the lesion was determined to be consistent with HCC. After multidisciplinary evaluation, he underwent microwave ablation with excellent response. Follow-up imaging 1- and 3-months later showed a treatment cavity with no findings of residual HCC (Figure 1). He continues to remain stable 2 years following treatment.
Discussion: Although the development of CFLD occurs in about 40% of CF patients, advanced liver disease has historically been less common with an incidence of about 10% by the age of 30 years. With recent CF treatment advances and longer life expectancies, the prevalence of adult CFLD has increased. HCC however has only been reported in 3 other cases thus far, all occurring in young patients between 18 and 34 years with high rates of advanced malignancy and mortality. Our case highlights the importance of close HCC surveillance of cirrhotic patients with CFLD, which can allow for early detection and timely treatment. Imaging and AFP every 6 months remains the standard of care. As therapeutic advances continue, the prevalence of adult CFLD and associated complications will increase, and clinicians must remain vigilant in this population.
Disclosures:
Rama Tarakji, MD1, Sunny Sandhu, MD2, Paul Martin, MD2. P2986 - Hepatocellular Carcinoma in Cirrhosis Due to Cystic Fibrosis Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mount Sinai Medical Center, Miami, FL; 2University of Miami Miller School of Medicine, Miami, FL
Introduction: Cystic fibrosis liver disease (CFLD) has been well-described in the pediatric population, however with increased life expectancy rates, a second wave has been observed in recent years in adults, and currently represents the third most common cause of death. Although complications from portal hypertension have been described in the setting of CFLD, the development of hepatocellular carcinoma (HCC) is an extremely rare event which has only described in 3 other cases. We present a patient with CFLD who developed HCC that was successfully treated with microwave ablation.
Case Description/Methods: A 36-year-old male with CF diagnosed at age 6, complicated by pancreatic exocrine insufficiency, pulmonary manifestations, and 10-year history of cirrhosis with ascites and non-bleeding esophageal varices, was under routine surveillance of CFLD. Laboratory studies showed ALT 19 U/L, AST 29 U/L, ALP 77 U/L, total bilirubin 0.6 mg/dL, albumin 3.7 g/dL, INR 1.1, alpha-fetoprotein (AFP) 1.4 ng/mL. CT triple-phase showed a new LI-RADS 3, 1cm arterial hyper-enhancing nodule in segment 7. Close interval imaging 3 months later showed a LI-RADS 4 lesion with interval growth to 1.2cm with arterial enhancement and washout on delayed imaging (Figure 1). Given the short-interval growth and concerning imaging findings in the setting of long-standing cirrhosis, the lesion was determined to be consistent with HCC. After multidisciplinary evaluation, he underwent microwave ablation with excellent response. Follow-up imaging 1- and 3-months later showed a treatment cavity with no findings of residual HCC (Figure 1). He continues to remain stable 2 years following treatment.
Discussion: Although the development of CFLD occurs in about 40% of CF patients, advanced liver disease has historically been less common with an incidence of about 10% by the age of 30 years. With recent CF treatment advances and longer life expectancies, the prevalence of adult CFLD has increased. HCC however has only been reported in 3 other cases thus far, all occurring in young patients between 18 and 34 years with high rates of advanced malignancy and mortality. Our case highlights the importance of close HCC surveillance of cirrhotic patients with CFLD, which can allow for early detection and timely treatment. Imaging and AFP every 6 months remains the standard of care. As therapeutic advances continue, the prevalence of adult CFLD and associated complications will increase, and clinicians must remain vigilant in this population.
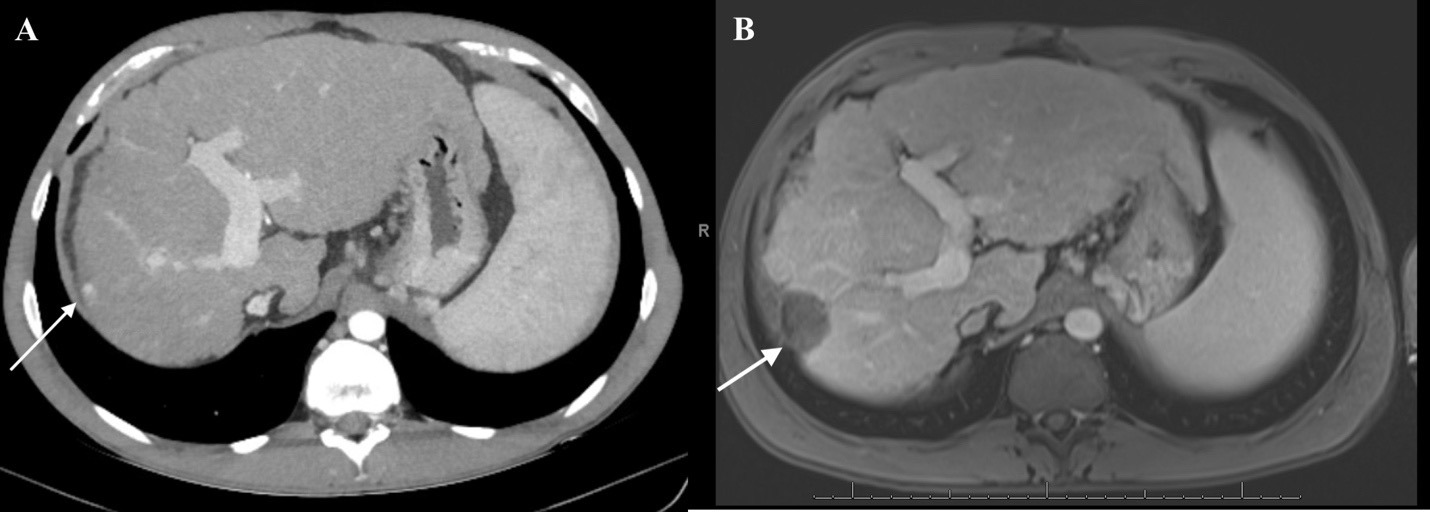
Figure: Figure 1: (A): CT abdomen with and without contrast demonstrating a 1.2cm arterially enhancing nodule in hepatic segment 7 demonstrating washout on delayed imaging, concerning for hepatocellular carcinoma. (B): Follow-up MRI abdomen with and without contrast, 3 months after ablation, demonstrating cirrhotic liver morphology with sequela portal hypertension, and new treatment cavity in segment 7 without findings of new or residual HCC.
Disclosures:
Rama Tarakji indicated no relevant financial relationships.
Sunny Sandhu indicated no relevant financial relationships.
Paul Martin indicated no relevant financial relationships.
Rama Tarakji, MD1, Sunny Sandhu, MD2, Paul Martin, MD2. P2986 - Hepatocellular Carcinoma in Cirrhosis Due to Cystic Fibrosis Liver Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
