Monday Poster Session
Category: Liver
P3009 - Infiltrative Liver Disease: A Case of Hepatic AL Amyloidosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Katrina Carolyn Soyangco, MD
University of Iowa Hospitals & Clinics
Iowa City, IA
Presenting Author(s)
Katrina Carolyn Soyangco, MD1, Alexander A. Garza, MD1, Alan Gunderson, MD2, Alex Cuskey, MD1, Matthew Gosse, MD1
1University of Iowa Hospitals & Clinics, Iowa City, IA; 2University of Iowa, Iowa City, IA
Introduction: Amyloidosis is an infiltrative disease characterized by deposition of amyloid in organs including the liver. This can lead to organ dysfunction, failure, and death. Hepatic amyloidosis can present with nonspecific signs and symptoms, making diagnosis elusive.
Case Description/Methods: A 75-year-old man presented with worsening liver chemistries over 16 months. The patient had a history of rheumatoid arthritis, interstitial lung disease on nintedanib, and chronic kidney disease. The patient was recently diagnosed with atrial fibrillation and underwent pacemaker placement for sinus node dysfunction. Exam showed scleral icterus and abdominal distention.
Laboratory studies were significant for ALP 595, ALT 38, AST 80, total and direct bilirubin 4.6 and 3.4, consistent with cholestatic liver injury. MRI abdomen revealed hepatomegaly, moderate ascites, and non-dilated bile ducts.
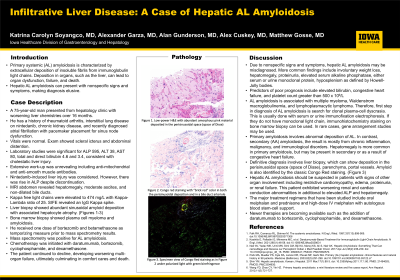
Extensive work-up was unrevealing including anti-mitochondrial and anti-smooth muscle antibodies. Nintedanib-induced liver injury was considered; however, there was rise in ALP despite discontinuation. Concern for systemic process, with worsening renal failure and recent cardiac conduction abnormalities, prompted further investigation. Kappa free light chains were elevated to 474 mg/L with Kappa-Lambda ratio of 25. SIFE revealed an IgG Kappa spike. Liver biopsy showed abundant sinusoidal amyloid deposition with associated hepatocyte atrophy. Bone marrow biopsy showed plasma cell myeloma and amyloidosis. Mass spectrometry was positive for AL amyloidosis. Chemotherapy was initiated with daratumumab, bortezomib, cyclophosphamide, and dexamethasone. The patient continued to decline, developing worsening multi-organ failure, ultimately culminating in comfort cares and death.
Discussion: Hepatic amyloidosis is a rare infiltrative liver disease that can cause abnormal liver chemistries. AL amyloidosis a plasma cell disease with results found secondarily in other organs, unlike the more common familial amyloidosis. Patients usually present with elevated ALP and hepatomegaly. The disease portends a poor prognosis. Due to nonspecific signs and symptoms, it can be misdiagnosed. Diagnosis of amyloidosis requires tissue biopsy to confirm presence of amyloid deposits in the liver by Congo Red staining, which classically shows green birefringence under polarized light. Hepatic amyloidosis should be suspected in patients with signs of other organ involvement including restrictive cardiomyopathy, edema, proteinuria, or renal failure.

Disclosures:
Katrina Carolyn Soyangco, MD1, Alexander A. Garza, MD1, Alan Gunderson, MD2, Alex Cuskey, MD1, Matthew Gosse, MD1. P3009 - Infiltrative Liver Disease: A Case of Hepatic AL Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Iowa Hospitals & Clinics, Iowa City, IA; 2University of Iowa, Iowa City, IA
Introduction: Amyloidosis is an infiltrative disease characterized by deposition of amyloid in organs including the liver. This can lead to organ dysfunction, failure, and death. Hepatic amyloidosis can present with nonspecific signs and symptoms, making diagnosis elusive.
Case Description/Methods: A 75-year-old man presented with worsening liver chemistries over 16 months. The patient had a history of rheumatoid arthritis, interstitial lung disease on nintedanib, and chronic kidney disease. The patient was recently diagnosed with atrial fibrillation and underwent pacemaker placement for sinus node dysfunction. Exam showed scleral icterus and abdominal distention.
Laboratory studies were significant for ALP 595, ALT 38, AST 80, total and direct bilirubin 4.6 and 3.4, consistent with cholestatic liver injury. MRI abdomen revealed hepatomegaly, moderate ascites, and non-dilated bile ducts.
Extensive work-up was unrevealing including anti-mitochondrial and anti-smooth muscle antibodies. Nintedanib-induced liver injury was considered; however, there was rise in ALP despite discontinuation. Concern for systemic process, with worsening renal failure and recent cardiac conduction abnormalities, prompted further investigation. Kappa free light chains were elevated to 474 mg/L with Kappa-Lambda ratio of 25. SIFE revealed an IgG Kappa spike. Liver biopsy showed abundant sinusoidal amyloid deposition with associated hepatocyte atrophy. Bone marrow biopsy showed plasma cell myeloma and amyloidosis. Mass spectrometry was positive for AL amyloidosis. Chemotherapy was initiated with daratumumab, bortezomib, cyclophosphamide, and dexamethasone. The patient continued to decline, developing worsening multi-organ failure, ultimately culminating in comfort cares and death.
Discussion: Hepatic amyloidosis is a rare infiltrative liver disease that can cause abnormal liver chemistries. AL amyloidosis a plasma cell disease with results found secondarily in other organs, unlike the more common familial amyloidosis. Patients usually present with elevated ALP and hepatomegaly. The disease portends a poor prognosis. Due to nonspecific signs and symptoms, it can be misdiagnosed. Diagnosis of amyloidosis requires tissue biopsy to confirm presence of amyloid deposits in the liver by Congo Red staining, which classically shows green birefringence under polarized light. Hepatic amyloidosis should be suspected in patients with signs of other organ involvement including restrictive cardiomyopathy, edema, proteinuria, or renal failure.

Figure: AL Amyloidosis of the Liver Pathology
Disclosures:
Katrina Carolyn Soyangco indicated no relevant financial relationships.
Alexander Garza indicated no relevant financial relationships.
Alan Gunderson indicated no relevant financial relationships.
Alex Cuskey indicated no relevant financial relationships.
Matthew Gosse indicated no relevant financial relationships.
Katrina Carolyn Soyangco, MD1, Alexander A. Garza, MD1, Alan Gunderson, MD2, Alex Cuskey, MD1, Matthew Gosse, MD1. P3009 - Infiltrative Liver Disease: A Case of Hepatic AL Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
