Monday Poster Session
Category: Liver
P3010 - Puzzling Peritonitis: Unraveling Ascitic Mysteries of Pelvic Inflammatory Disease
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

GRACE Lavandowksa, MD
University of North Dakota, School of Medicine and Health Sciences
Fargo, ND
Presenting Author(s)
GRACE Lavandowksa, MD1, Guneet Sidhu, MD2, John Bassett, MD, FACG3, Laura Nichols, MD3
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2University of North Dakota, Fargo, ND; 3Sanford Health, Fargo, ND
Introduction: Pelvic inflammatory disease (PID) is an infection primarily affecting the upper genital tract, involving the uterus, fallopian tubes, and ovaries. Common pathogens include Neisseria gonorrhea, Chlamydia trachomatis, and Mycoplasma genitalium. PID can manifest with diverse symptoms, leading to misdiagnosis. Ascites, a rare complication of PID, poses diagnostic challenges due to its diverse etiologies.
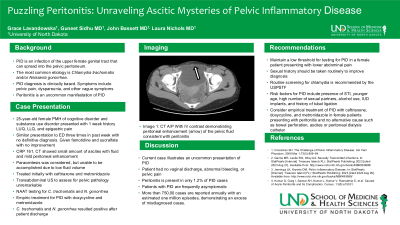
Case Description/Methods: A 25-year-old female with a history of cognitive disorder and substance use disorder was admitted with 7 days of left upper and lower quadrant pain. She denied fever, chills, nausea, vomiting, urinary symptoms, or bowel issues but exhibited abdominal distension upon examination. She presented to the ER on three occasions in the preceding week without receiving a definitive diagnosis. Negative workup in the ER included RUQ quadrant ultrasound as well as laboratory evaluation. Upon admission, her CBC, CMP, and lactic were normal, but CRP was elevated at 161.0 mg/L, indicative of an underlying inflammatory process. A CT scan of the abdomen unveiled ascites in the perihepatic/subhepatic, right paracolic gutter, and pelvic regions, with mild peritoneal enhancement. Diagnosed with peritonitis, she was initiated on IV ceftriaxone and metronidazole initially. The patient denied any significant alcohol use and did not exhibit clinical or laboratory evidence of cirrhosis. She denied recent sexual activity. Pelvic US to further define the pelvic fluid was unrevealing. Chlamydia trachomatis and Neisseria gonorrhea was pursued due to the lack of a definitive diagnosis. Infectious disease was consulted and treatment for PID was initiated. The patient was discharged with a 14-day course of doxycycline and metronidazole. Post-discharge testing revealed positive results for both C. trachomatis and N. gonorrhea, implicating them as the direct cause of her peritonitis and recurrent ER visits.
Discussion: Peritonitis, particularly with associated ascites, in PID cases is rare, but our case underscores the importance of considering PID in the differential diagnosis of undiagnosed abdominal pain, peritonitis and ascites, especially in young women. Chlamydia-induced ascites, although rare, should not be overlooked due to its potential long-term consequences. Awareness of uncommon presentations of PID can aid in prompt diagnosis and management, preventing long-term sequelae associated with untreated infections
Disclosures:
GRACE Lavandowksa, MD1, Guneet Sidhu, MD2, John Bassett, MD, FACG3, Laura Nichols, MD3. P3010 - Puzzling Peritonitis: Unraveling Ascitic Mysteries of Pelvic Inflammatory Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of North Dakota, School of Medicine and Health Sciences, Fargo, ND; 2University of North Dakota, Fargo, ND; 3Sanford Health, Fargo, ND
Introduction: Pelvic inflammatory disease (PID) is an infection primarily affecting the upper genital tract, involving the uterus, fallopian tubes, and ovaries. Common pathogens include Neisseria gonorrhea, Chlamydia trachomatis, and Mycoplasma genitalium. PID can manifest with diverse symptoms, leading to misdiagnosis. Ascites, a rare complication of PID, poses diagnostic challenges due to its diverse etiologies.
Case Description/Methods: A 25-year-old female with a history of cognitive disorder and substance use disorder was admitted with 7 days of left upper and lower quadrant pain. She denied fever, chills, nausea, vomiting, urinary symptoms, or bowel issues but exhibited abdominal distension upon examination. She presented to the ER on three occasions in the preceding week without receiving a definitive diagnosis. Negative workup in the ER included RUQ quadrant ultrasound as well as laboratory evaluation. Upon admission, her CBC, CMP, and lactic were normal, but CRP was elevated at 161.0 mg/L, indicative of an underlying inflammatory process. A CT scan of the abdomen unveiled ascites in the perihepatic/subhepatic, right paracolic gutter, and pelvic regions, with mild peritoneal enhancement. Diagnosed with peritonitis, she was initiated on IV ceftriaxone and metronidazole initially. The patient denied any significant alcohol use and did not exhibit clinical or laboratory evidence of cirrhosis. She denied recent sexual activity. Pelvic US to further define the pelvic fluid was unrevealing. Chlamydia trachomatis and Neisseria gonorrhea was pursued due to the lack of a definitive diagnosis. Infectious disease was consulted and treatment for PID was initiated. The patient was discharged with a 14-day course of doxycycline and metronidazole. Post-discharge testing revealed positive results for both C. trachomatis and N. gonorrhea, implicating them as the direct cause of her peritonitis and recurrent ER visits.
Discussion: Peritonitis, particularly with associated ascites, in PID cases is rare, but our case underscores the importance of considering PID in the differential diagnosis of undiagnosed abdominal pain, peritonitis and ascites, especially in young women. Chlamydia-induced ascites, although rare, should not be overlooked due to its potential long-term consequences. Awareness of uncommon presentations of PID can aid in prompt diagnosis and management, preventing long-term sequelae associated with untreated infections
Disclosures:
GRACE Lavandowksa indicated no relevant financial relationships.
Guneet Sidhu indicated no relevant financial relationships.
John Bassett indicated no relevant financial relationships.
Laura Nichols indicated no relevant financial relationships.
GRACE Lavandowksa, MD1, Guneet Sidhu, MD2, John Bassett, MD, FACG3, Laura Nichols, MD3. P3010 - Puzzling Peritonitis: Unraveling Ascitic Mysteries of Pelvic Inflammatory Disease, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
