Monday Poster Session
Category: Liver
P3011 - Hepatic Portosystemic Shunts in Non-Cirrhotic Patients on CT: A Case Series
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kirsten Loscalzo, MD
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Kirsten Loscalzo, MD1, Ghada Issa, MD2, Yousef Elfanagely, MD2, Laura Massa, ANPC3, Fadlallah Habr, MD4
1Brown University / Rhode Island Hospital, Providence, RI; 2Lifespan Health System, Providence, RI; 3Brown University / Lifespan Physician Group, Providence, RI; 4Rhode Island Hospital, Providence, RI
Introduction: We present 2 cases of portosystemic shunts in non-cirrhotic patients found incidentally on abdominal CT. Non-cirrhotic portosystemic shunts are very rare with one study suggesting a prevalence of 0.02% in patients undergoing abdominal imaging. There is little literature regarding when to surgically correct these shunts.
Case Description/Methods: Cases were identified by our radiologist on routine reads of abdominal CT scans.
Case 1 is a 65-year-old female with irritable bowel disease and gastroesophageal reflux disease who presented for a 4 phase CT scan of the liver for possible aorto-venous (AV) fistula of the right hepatic lobe seen on RUQ ultrasound. The initial ultrasound was done for workup of metabolic dysfunction-associated steatotic liver disease. Ultimately she was found not to have an AV fistula, and instead had an incidental portosystemic shunt. Given the shunt, a fibroscan was completed that showed no evidence of cirrhosis. Patient reported she had no history of biliary drains, liver biopsy or significant abdominal trauma. She has no documented autoimmune or vasculitic disease.
Case 2 is an 82-year-old male with anxiety and depression who presented with a femur fracture that was managed non-operatively given significant comorbidities. While hospitalized he underwent CT for abdominal pain and was found to have Ogilvie's syndrome and a small porto-systemic shunt in the right hepatic lobe with no cirrhotic morphology. Throughout his hospitalization he was intermittently confused. There was no documented history of cirrhosis, biliary drains or liver biopsy.
Both cases had normal baseline AST, ALT, alkaline phosphatase, total bilirubin, direct bilirubin and platelet count. In Case 1 PT and INR were within normal limits. In Case 2, PT and INR were elevated in the setting of warfarin use. Neither of our patients received surgery for these portosystemic shunts, although one of our patients was potentially symptomatic from the shunt given his intermittent confusion and elevated INR.
Discussion: We identified portosystemic shunts in two non-cirrhotic patients, a rare condition, found incidentally on abdominal CT. The current literature does show these shunts can progress to become clinically significant and cause hyperammonemia, mood disorders or hepatic encephalopathy. Symptoms can resolved with shunt repair. Further research is needed to better understand when these patients might benefit from prophylactic surgical correction and when surgery is not needed.
Disclosures:
Kirsten Loscalzo, MD1, Ghada Issa, MD2, Yousef Elfanagely, MD2, Laura Massa, ANPC3, Fadlallah Habr, MD4. P3011 - Hepatic Portosystemic Shunts in Non-Cirrhotic Patients on CT: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2Lifespan Health System, Providence, RI; 3Brown University / Lifespan Physician Group, Providence, RI; 4Rhode Island Hospital, Providence, RI
Introduction: We present 2 cases of portosystemic shunts in non-cirrhotic patients found incidentally on abdominal CT. Non-cirrhotic portosystemic shunts are very rare with one study suggesting a prevalence of 0.02% in patients undergoing abdominal imaging. There is little literature regarding when to surgically correct these shunts.
Case Description/Methods: Cases were identified by our radiologist on routine reads of abdominal CT scans.
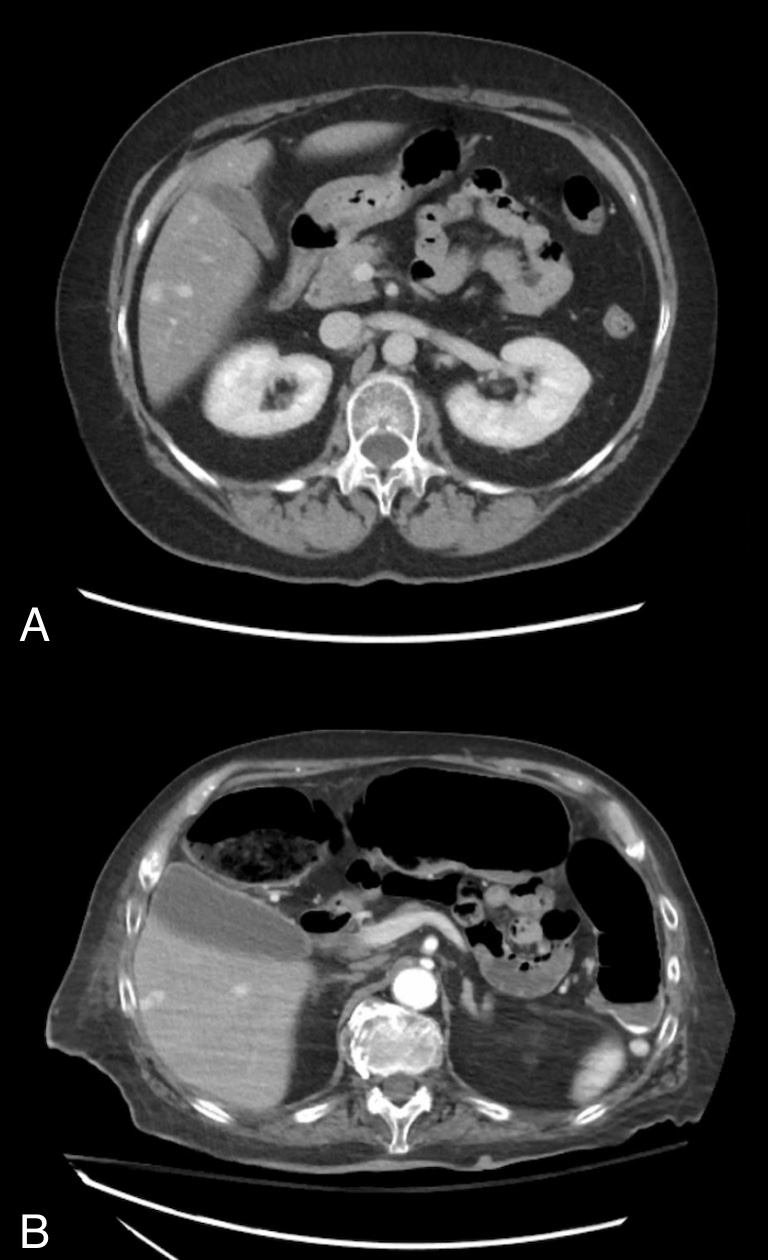
Case 1 is a 65-year-old female with irritable bowel disease and gastroesophageal reflux disease who presented for a 4 phase CT scan of the liver for possible aorto-venous (AV) fistula of the right hepatic lobe seen on RUQ ultrasound. The initial ultrasound was done for workup of metabolic dysfunction-associated steatotic liver disease. Ultimately she was found not to have an AV fistula, and instead had an incidental portosystemic shunt. Given the shunt, a fibroscan was completed that showed no evidence of cirrhosis. Patient reported she had no history of biliary drains, liver biopsy or significant abdominal trauma. She has no documented autoimmune or vasculitic disease.
Case 2 is an 82-year-old male with anxiety and depression who presented with a femur fracture that was managed non-operatively given significant comorbidities. While hospitalized he underwent CT for abdominal pain and was found to have Ogilvie's syndrome and a small porto-systemic shunt in the right hepatic lobe with no cirrhotic morphology. Throughout his hospitalization he was intermittently confused. There was no documented history of cirrhosis, biliary drains or liver biopsy.
Both cases had normal baseline AST, ALT, alkaline phosphatase, total bilirubin, direct bilirubin and platelet count. In Case 1 PT and INR were within normal limits. In Case 2, PT and INR were elevated in the setting of warfarin use. Neither of our patients received surgery for these portosystemic shunts, although one of our patients was potentially symptomatic from the shunt given his intermittent confusion and elevated INR.
Discussion: We identified portosystemic shunts in two non-cirrhotic patients, a rare condition, found incidentally on abdominal CT. The current literature does show these shunts can progress to become clinically significant and cause hyperammonemia, mood disorders or hepatic encephalopathy. Symptoms can resolved with shunt repair. Further research is needed to better understand when these patients might benefit from prophylactic surgical correction and when surgery is not needed.
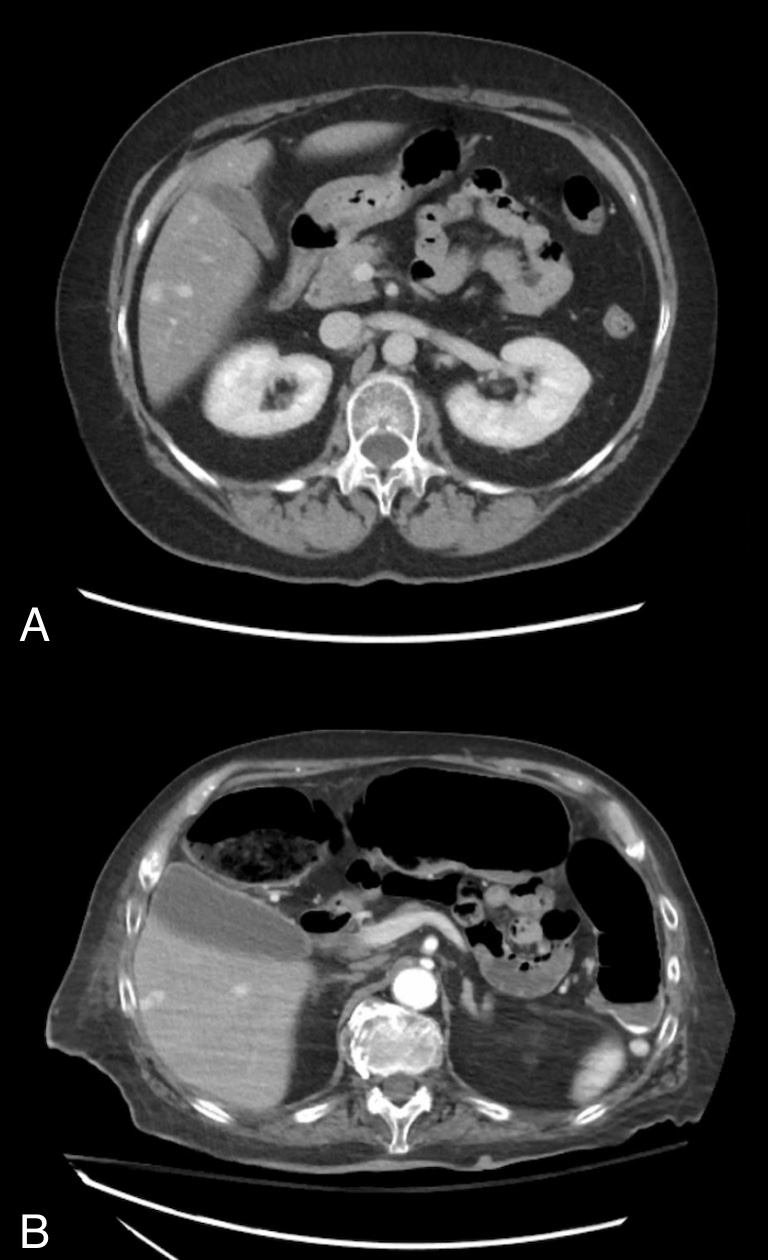
Figure: A: Intrahepatic portosystemic shunt within the right hepatic lobe, between the right hepatic vein and the right anterior portal vein.
B: Small portosystemic shunt in the right hepatic lobe.
B: Small portosystemic shunt in the right hepatic lobe.
Disclosures:
Kirsten Loscalzo indicated no relevant financial relationships.
Ghada Issa indicated no relevant financial relationships.
Yousef Elfanagely indicated no relevant financial relationships.
Laura Massa indicated no relevant financial relationships.
Fadlallah Habr indicated no relevant financial relationships.
Kirsten Loscalzo, MD1, Ghada Issa, MD2, Yousef Elfanagely, MD2, Laura Massa, ANPC3, Fadlallah Habr, MD4. P3011 - Hepatic Portosystemic Shunts in Non-Cirrhotic Patients on CT: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

