Monday Poster Session
Category: Liver
P3034 - A Pregnancy Puzzle: Severe Acute Hepatitis Secondary to Peripartum Hemophagocytic Lymphohistiocytosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Areeba Khwaja, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Areeba Khwaja, MD, Akshata Moghe, MD, PhD
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a life-threatening syndrome of hyper-immunity resulting in multi-organ damage. It is extremely rare in the peripartum population. Acute liver injury is known to be a common complication of HLH. Given that HLH may cause fulminant liver failure requiring urgent transplantation in pregnant women as well as growth restriction, stillbirth, and even fetal demise for the fetus, timely recognition and intervention is key.
Case Description/Methods: A previously healthy 38 year-old G5P1 pregnant woman at 20 weeks gestation was transferred from an outside hospital with jaundice, scleral icterus, and generalized abdominal pain of several days duration. Initial labs were notable for AST of 5780 U/L, ALT of 2471 U/L, alkaline phosphatase of 142 U/L, total bilirubin of 12 mg/dL, and ferritin >40,000 ng/mL. INR was normal and no mental deficits were present. The patient denied any recent travel or drug ingestion, labs were inconsistent with acute viral hepatitis, and there was no concern for ischemia. Findings were inconsistent with HELLP Syndrome or cholestasis of pregnancy. Chronic liver disease, autoimmune, and broad infectious workups were initiated. Imaging demonstrated gallstones but no biliary dilatation or choledocholithiasis. The patient was empirically started on N-Acetylcysteine, broad-spectrum antibiotics, and treatment for HSV hepatitis, which can cause idiopathic fulminant hepatitis particularly in pregnancy. On day 2 of hospitalization, the patient underwent liver biopsy. Thereafter, she deferred etoposide but agreed to start empiric intravenous dexamethasone. By day 3, liver enzymes began to downtrend and biopsy results confirmed diagnosis of HLH as per the clinical criteria listed in Table 1. All other work-up remained unremarkable. On day 10, after continued decline in ferritin and liver enzymes while on steroid therapy, the patient was discharged and subsequently completed her taper outpatient with close follow-up. She delivered a healthy female infant at 36 weeks without complication.
Discussion: There should be a high index of suspicion for HLH and prompt initiation of treatment for patients presenting with acute hepatitis of unclear etiology, including pregnant women. Current guidelines for HLH are limited to studies from the pediatric population. Guidelines for adult patients would be beneficial in navigating treatment options, including steroid therapy and chemotherapeutic agents, especially for patient populations vulnerable to poor outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Areeba Khwaja, MD, Akshata Moghe, MD, PhD. P3034 - A Pregnancy Puzzle: Severe Acute Hepatitis Secondary to Peripartum Hemophagocytic Lymphohistiocytosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas Health, McGovern Medical School, Houston, TX
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a life-threatening syndrome of hyper-immunity resulting in multi-organ damage. It is extremely rare in the peripartum population. Acute liver injury is known to be a common complication of HLH. Given that HLH may cause fulminant liver failure requiring urgent transplantation in pregnant women as well as growth restriction, stillbirth, and even fetal demise for the fetus, timely recognition and intervention is key.
Case Description/Methods: A previously healthy 38 year-old G5P1 pregnant woman at 20 weeks gestation was transferred from an outside hospital with jaundice, scleral icterus, and generalized abdominal pain of several days duration. Initial labs were notable for AST of 5780 U/L, ALT of 2471 U/L, alkaline phosphatase of 142 U/L, total bilirubin of 12 mg/dL, and ferritin >40,000 ng/mL. INR was normal and no mental deficits were present. The patient denied any recent travel or drug ingestion, labs were inconsistent with acute viral hepatitis, and there was no concern for ischemia. Findings were inconsistent with HELLP Syndrome or cholestasis of pregnancy. Chronic liver disease, autoimmune, and broad infectious workups were initiated. Imaging demonstrated gallstones but no biliary dilatation or choledocholithiasis. The patient was empirically started on N-Acetylcysteine, broad-spectrum antibiotics, and treatment for HSV hepatitis, which can cause idiopathic fulminant hepatitis particularly in pregnancy. On day 2 of hospitalization, the patient underwent liver biopsy. Thereafter, she deferred etoposide but agreed to start empiric intravenous dexamethasone. By day 3, liver enzymes began to downtrend and biopsy results confirmed diagnosis of HLH as per the clinical criteria listed in Table 1. All other work-up remained unremarkable. On day 10, after continued decline in ferritin and liver enzymes while on steroid therapy, the patient was discharged and subsequently completed her taper outpatient with close follow-up. She delivered a healthy female infant at 36 weeks without complication.
Discussion: There should be a high index of suspicion for HLH and prompt initiation of treatment for patients presenting with acute hepatitis of unclear etiology, including pregnant women. Current guidelines for HLH are limited to studies from the pediatric population. Guidelines for adult patients would be beneficial in navigating treatment options, including steroid therapy and chemotherapeutic agents, especially for patient populations vulnerable to poor outcomes.
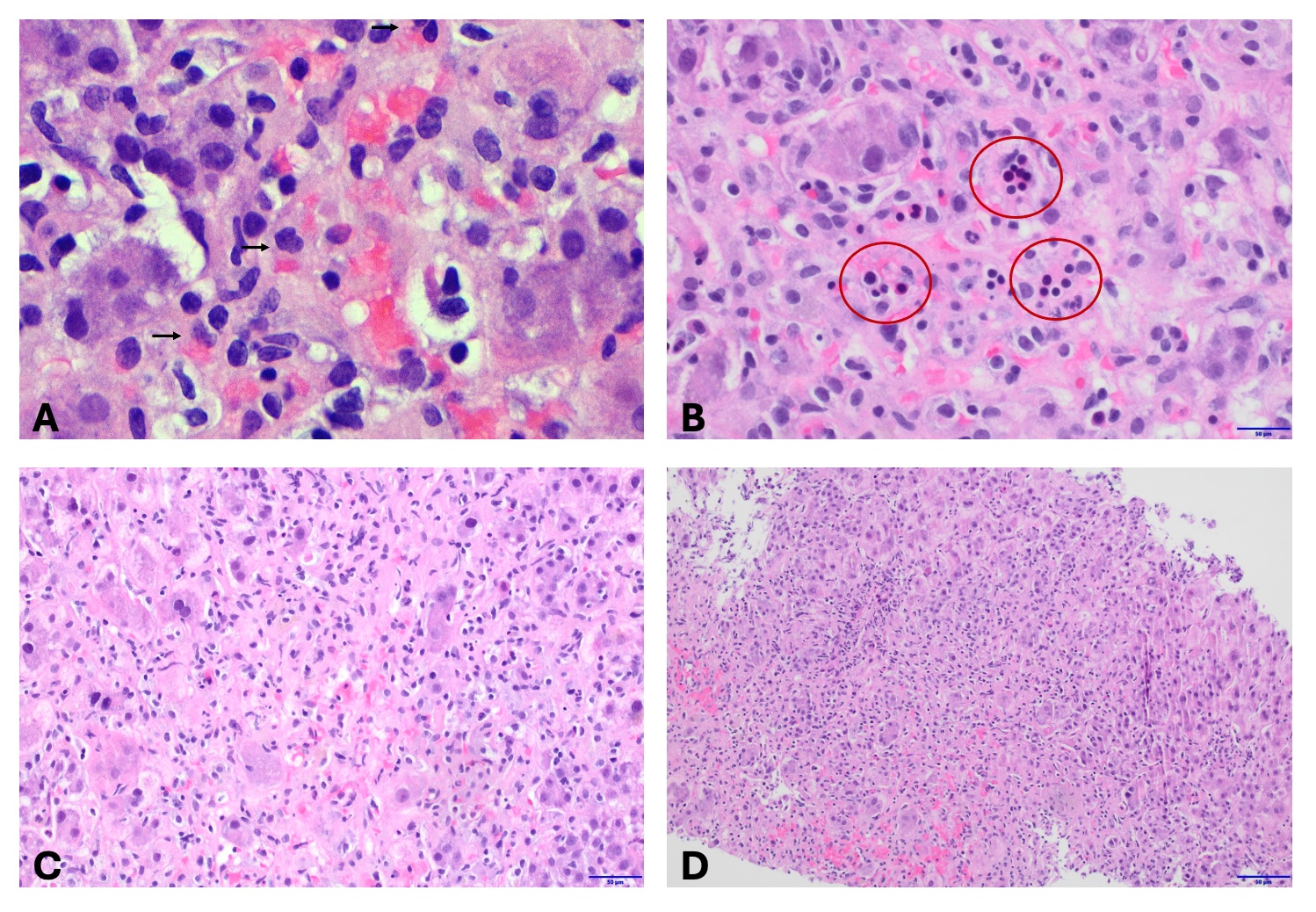
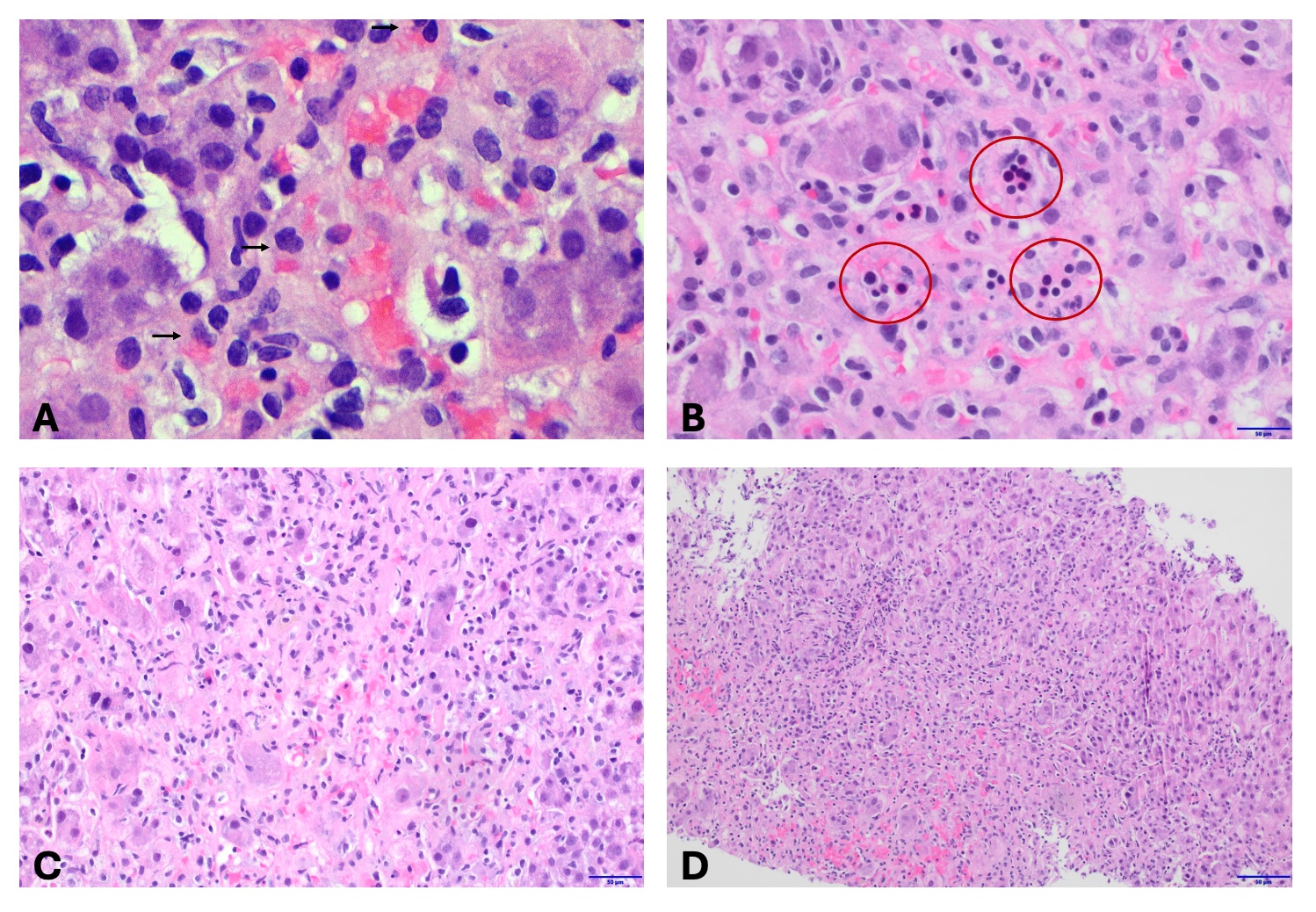
Figure: Figure 1. Microscopic examination from the patient's liver biopsy shows an acute hepatitis pattern with diffuse lobular disarray, scattered lobular inflammation, and hepatocyte damage.
A. Hepatic parenchyma with scattered macrophages containing red blood cells (see arrows) as well as scattered admixed lymphocytes [H&E, 500x].
B. Extra-medullary hematopoiesis in hepatic parenchyma [H&E, 40x].
C. Focal hepatocyte necrosis replaced by inflammation (macrophages, lymphocytes, and neutrophils) [H&E, 20x].
D. Normal lobular architecture that is disrupted by hepatocyte injury and inflammation [H&E, 10x].
A. Hepatic parenchyma with scattered macrophages containing red blood cells (see arrows) as well as scattered admixed lymphocytes [H&E, 500x].
B. Extra-medullary hematopoiesis in hepatic parenchyma [H&E, 40x].
C. Focal hepatocyte necrosis replaced by inflammation (macrophages, lymphocytes, and neutrophils) [H&E, 20x].
D. Normal lobular architecture that is disrupted by hepatocyte injury and inflammation [H&E, 10x].
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Areeba Khwaja indicated no relevant financial relationships.
Akshata Moghe: Alnylam – Consultant. Recordati Rare Dis Inc. – Consultant.
Areeba Khwaja, MD, Akshata Moghe, MD, PhD. P3034 - A Pregnancy Puzzle: Severe Acute Hepatitis Secondary to Peripartum Hemophagocytic Lymphohistiocytosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
