Monday Poster Session
Category: Liver
P3035 - Atypical Late Presentations of Metastatic Hepatocellular Carcinoma After Liver Transplant
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Yara JN Dababneh, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Yara JN. Dababneh, MD1, Reena J. Salgia, MD2
1Henry Ford Health, Detroit, MI; 2Henry Ford Medical Group, Henry Ford Health System, Detroit, MI
Introduction: Liver transplantation (LT) is the primary curative option for hepatocellular carcinoma (HCC). Two cases here exemplify late and atypical metastatic HCC post-LT.
Case Description/Methods: Case 1: 67-year-old female with a history of Hepatitis C (HCV) cirrhosis complicated by HCC underwent liver transplantation in 2011. She received pre-transplant treatment. Pathology results of the explanted liver revealed 4.5 cm well-differentiated HCC without evidence of any invasion.Post-LT, the patient underwent routine surveillance every six months for five years. Elevated AFP was noted incidentally 12 years post-LT which led to the discovery of metastatic HCC in the right mesorectal fascia. During surgery an ovoid peritoneal metastasis was found and excised. Pathology revealed moderately differentiated HCC. Despite initiation of tyrosine kinase inhibitor (TKI) therapy, AFP levels exhibited resurgence. Continued surveillance revealed the presence of a new adnexal mass prompting bilateral salpingo-oophorectomy, which confirmed metastatic HCC. Following surgery, AFP levels demonstrated a decline. Case 2:71-year-old male with a history of HCV cirrhosis complicated by HCC underwent LT in 2006. Patient underwent pre-LT treatment. Pathology report of the explanted liver revealed a 3.5 cm moderately differentiated HCC without any invasion. Post-LT surveillance for recurrent HCC was conducted. However,15 years post-LT, AFP was noted incidentally to be elevated at 644 ng/ml. Despite negative initial imaging studies, subsequent surveillance identified two masses abutting the sigmoid colon. Biopsy confirmed metastatic HCC. The patient was initiated on TKI-based therapy, with plans for surgery, which revealed extensive peritoneal carcinomatosis. Biopsy confirmed metastatic HCC. Despite therapeutic interventions, AFP levels continued to rise, prompting a shift to second and subsequently third-line systemic therapy. Notably, due to disease progression, patient opted for immune checkpoint inhibitor therapy, which was discontinued due to graft rejection.
Discussion: These cases demonstrate the challenges with post-LT HCC recurrence. Post-LT surveillance entails imaging studies and AFP assessments up to five years. Elevated AFP beyond this period warrants pelvic imaging if standard scans are inconclusive. The feasibility of continued AFP monitoring beyond 5 years needs further research. In summary, late and atypical HCC recurrence post-LT calls for the need for innovative diagnostic approaches to enhance patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yara JN. Dababneh, MD1, Reena J. Salgia, MD2. P3035 - Atypical Late Presentations of Metastatic Hepatocellular Carcinoma After Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2Henry Ford Medical Group, Henry Ford Health System, Detroit, MI
Introduction: Liver transplantation (LT) is the primary curative option for hepatocellular carcinoma (HCC). Two cases here exemplify late and atypical metastatic HCC post-LT.
Case Description/Methods: Case 1: 67-year-old female with a history of Hepatitis C (HCV) cirrhosis complicated by HCC underwent liver transplantation in 2011. She received pre-transplant treatment. Pathology results of the explanted liver revealed 4.5 cm well-differentiated HCC without evidence of any invasion.Post-LT, the patient underwent routine surveillance every six months for five years. Elevated AFP was noted incidentally 12 years post-LT which led to the discovery of metastatic HCC in the right mesorectal fascia. During surgery an ovoid peritoneal metastasis was found and excised. Pathology revealed moderately differentiated HCC. Despite initiation of tyrosine kinase inhibitor (TKI) therapy, AFP levels exhibited resurgence. Continued surveillance revealed the presence of a new adnexal mass prompting bilateral salpingo-oophorectomy, which confirmed metastatic HCC. Following surgery, AFP levels demonstrated a decline. Case 2:71-year-old male with a history of HCV cirrhosis complicated by HCC underwent LT in 2006. Patient underwent pre-LT treatment. Pathology report of the explanted liver revealed a 3.5 cm moderately differentiated HCC without any invasion. Post-LT surveillance for recurrent HCC was conducted. However,15 years post-LT, AFP was noted incidentally to be elevated at 644 ng/ml. Despite negative initial imaging studies, subsequent surveillance identified two masses abutting the sigmoid colon. Biopsy confirmed metastatic HCC. The patient was initiated on TKI-based therapy, with plans for surgery, which revealed extensive peritoneal carcinomatosis. Biopsy confirmed metastatic HCC. Despite therapeutic interventions, AFP levels continued to rise, prompting a shift to second and subsequently third-line systemic therapy. Notably, due to disease progression, patient opted for immune checkpoint inhibitor therapy, which was discontinued due to graft rejection.
Discussion: These cases demonstrate the challenges with post-LT HCC recurrence. Post-LT surveillance entails imaging studies and AFP assessments up to five years. Elevated AFP beyond this period warrants pelvic imaging if standard scans are inconclusive. The feasibility of continued AFP monitoring beyond 5 years needs further research. In summary, late and atypical HCC recurrence post-LT calls for the need for innovative diagnostic approaches to enhance patient outcomes.
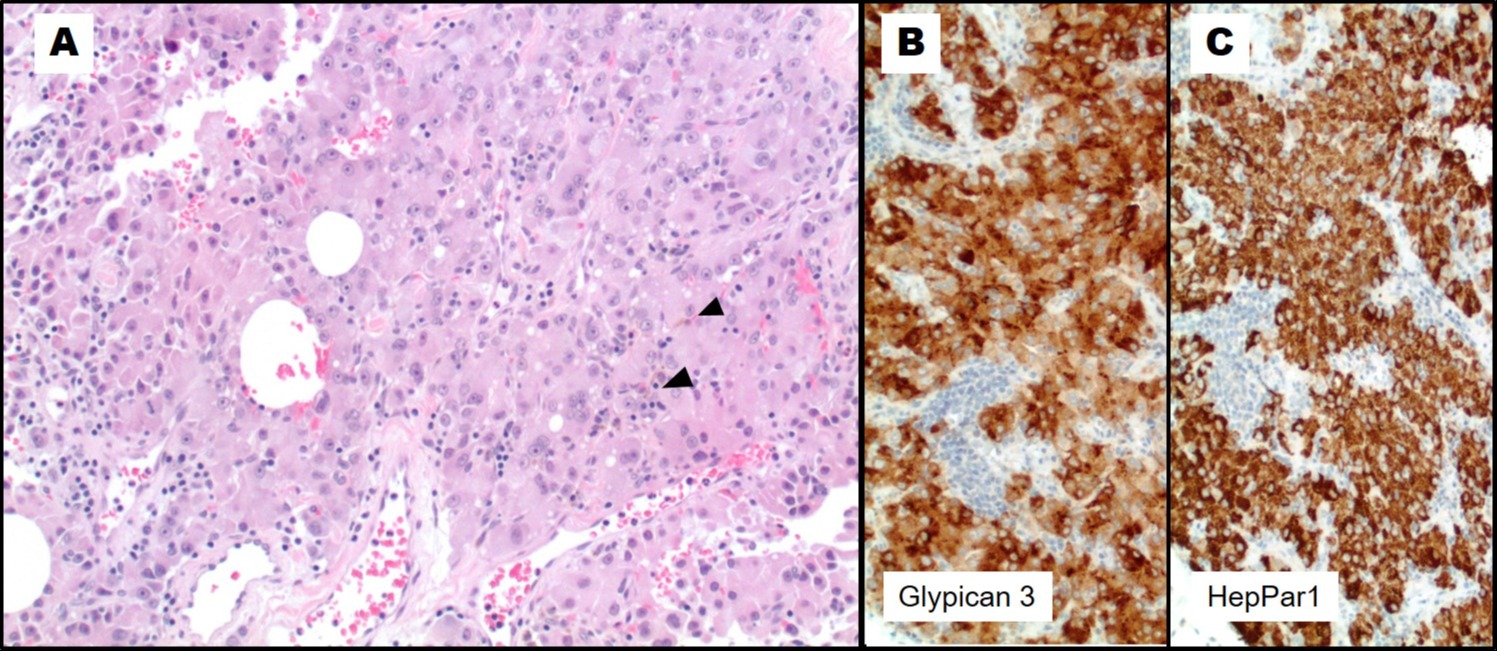
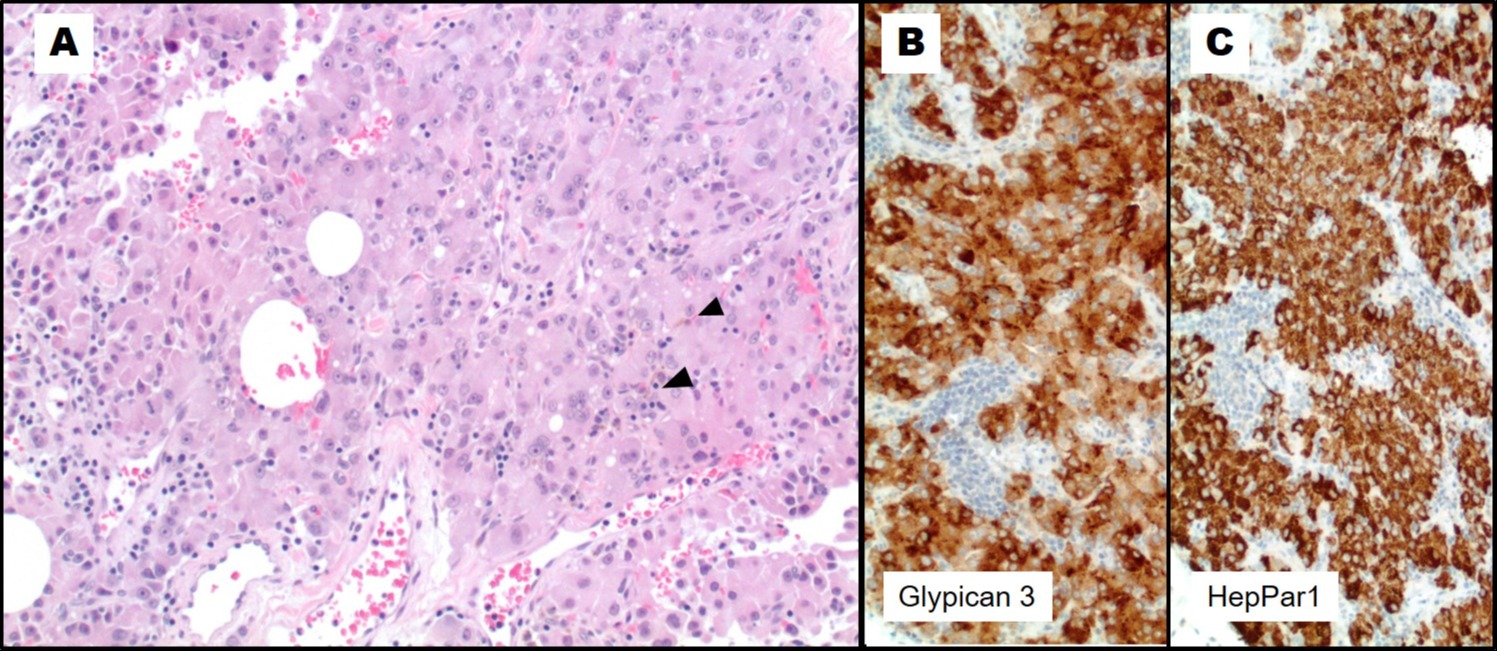
Figure: (A) The H&E-stained sections demonstrate a cellular proliferation composed of polygonal shaped cells with abundant eosinophilic granular cytoplasm, round nuclei with prominent nucleoli, intervening vasculature, scattered inflammatory cells and focal bile production (arrow heads). (B & C) Immunohistochemical staining demonstrates the lesional cells are diffusely positive for Glypican 3 and HepPar 1. Other site-specific markers are negative.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Yara Dababneh indicated no relevant financial relationships.
Reena Salgia: AstraZeneca – Advisor or Review Panel Member. Cook Medical – Educational video. Eisai – Speakers Bureau. Exelixis – Speakers Bureau.
Yara JN. Dababneh, MD1, Reena J. Salgia, MD2. P3035 - Atypical Late Presentations of Metastatic Hepatocellular Carcinoma After Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
