Monday Poster Session
Category: Liver
P3037 - Nephrogenic Ascites: A Rare Cause of Refractory Ascites
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Elona Poltiyelova, DO
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Elona Poltiyelova, DO, Aaron Schluger, MD, Virendra Tewari, MD, FACG
Westchester Medical Center, Valhalla, NY
Introduction: Nephrogenic ascites is a rare form of refractory ascites that can develop in patients with ESRD on hemodialysis. Understanding this condition is paramount for clinicians facing its diagnostic and therapeutic challenges, given its poor prognosis and limited treatment options. We present a case of nephrogenic ascites that highlights its complexity and diagnostic challenges.
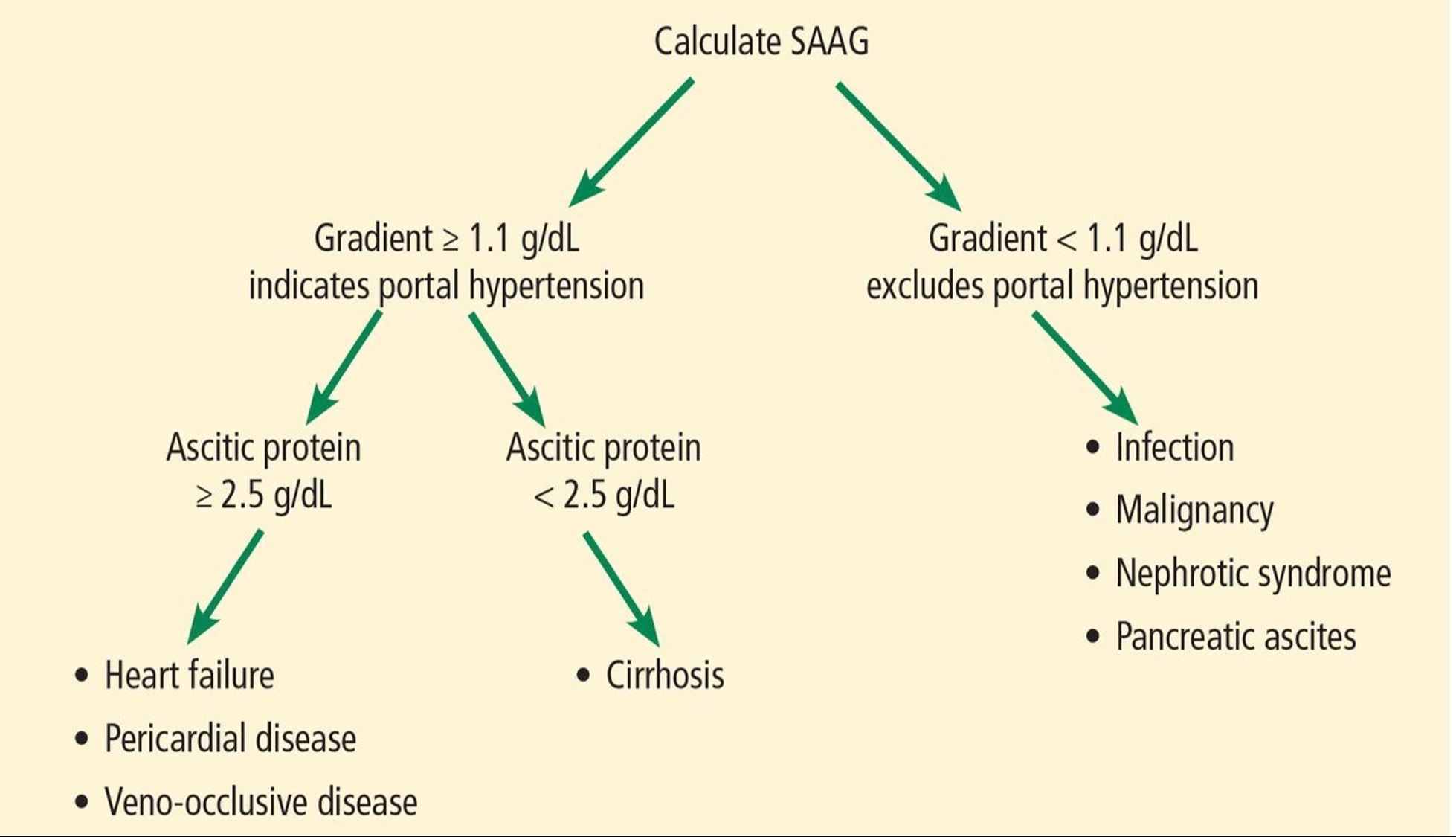
Case Description/Methods: A 73 year old man with ESRD (on hemodialysis), diabetes, and history of recurrent ascites presented with increasing abdominal distension. Ultrasound showed large volume ascites, with the absence of portal hypertension, and he received a paracentesis which drained 8L of yellow ascitic fluid. Fluid studies showed: total protein 3.8, albumin 1.8, WBC 351, 0% PMN, amylase 40, LDH 82, and was negative for Spontaneous Bacterial Peritonitis by cell count and fluid culture. The serum albumin ascites gradient (SAAG) was 0.9, like his other admissions. A low SAAG (< 1.1) and high protein ascites commonly signifies ascites due to peritoneal carcinomatosis, tuberculosis, pancreatic ascites, biliary ascites, or serositis. The patient had a normal echocardiogram and a negative ANA, AFB, QuantiFERON, adenosine deaminase, Hepatitis Panel, fungal culture, peritoneal biopsy, and fluid cytology.
After a detailed workup and excluding hepatic, cardiac, infectious and malignant causes of ascites, a diagnosis of nephrogenic ascites was made. Due to its refractory nature, the patient has been returning for the same complaint. He will be seen outpatient to determine if he is a candidate for renal transplantation.
Discussion: Nephrogenic ascites is a diagnosis of exclusion in patients with ESRD that are usually on hemodialysis, and is often refractory to conventional treatment. The pathophysiology is not fully understood but some theories include impaired lymphatic drainage and increased permeability of the peritoneal membrane due to uremic toxins. Patients usually present with low SAAG, low WBC, and high protein ascites. Management includes salt and fluid restriction, albumin infusion, and frequent paracentesis. However nephrogenic ascites remains difficult to control, with over a 40% mortality rate within 15 months of diagnosis. Kidney transplantation is the only definitive treatment, but not all patients are transplant candidates.
Nephrogenic ascites continues to present complex clinical dilemmas, therefore there is a need to spread awareness and for further research into its underlying mechanisms and management options.
Disclosures:
Elona Poltiyelova, DO, Aaron Schluger, MD, Virendra Tewari, MD, FACG. P3037 - Nephrogenic Ascites: A Rare Cause of Refractory Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Westchester Medical Center, Valhalla, NY
Introduction: Nephrogenic ascites is a rare form of refractory ascites that can develop in patients with ESRD on hemodialysis. Understanding this condition is paramount for clinicians facing its diagnostic and therapeutic challenges, given its poor prognosis and limited treatment options. We present a case of nephrogenic ascites that highlights its complexity and diagnostic challenges.
Case Description/Methods: A 73 year old man with ESRD (on hemodialysis), diabetes, and history of recurrent ascites presented with increasing abdominal distension. Ultrasound showed large volume ascites, with the absence of portal hypertension, and he received a paracentesis which drained 8L of yellow ascitic fluid. Fluid studies showed: total protein 3.8, albumin 1.8, WBC 351, 0% PMN, amylase 40, LDH 82, and was negative for Spontaneous Bacterial Peritonitis by cell count and fluid culture. The serum albumin ascites gradient (SAAG) was 0.9, like his other admissions. A low SAAG (< 1.1) and high protein ascites commonly signifies ascites due to peritoneal carcinomatosis, tuberculosis, pancreatic ascites, biliary ascites, or serositis. The patient had a normal echocardiogram and a negative ANA, AFB, QuantiFERON, adenosine deaminase, Hepatitis Panel, fungal culture, peritoneal biopsy, and fluid cytology.
After a detailed workup and excluding hepatic, cardiac, infectious and malignant causes of ascites, a diagnosis of nephrogenic ascites was made. Due to its refractory nature, the patient has been returning for the same complaint. He will be seen outpatient to determine if he is a candidate for renal transplantation.
Discussion: Nephrogenic ascites is a diagnosis of exclusion in patients with ESRD that are usually on hemodialysis, and is often refractory to conventional treatment. The pathophysiology is not fully understood but some theories include impaired lymphatic drainage and increased permeability of the peritoneal membrane due to uremic toxins. Patients usually present with low SAAG, low WBC, and high protein ascites. Management includes salt and fluid restriction, albumin infusion, and frequent paracentesis. However nephrogenic ascites remains difficult to control, with over a 40% mortality rate within 15 months of diagnosis. Kidney transplantation is the only definitive treatment, but not all patients are transplant candidates.
Nephrogenic ascites continues to present complex clinical dilemmas, therefore there is a need to spread awareness and for further research into its underlying mechanisms and management options.
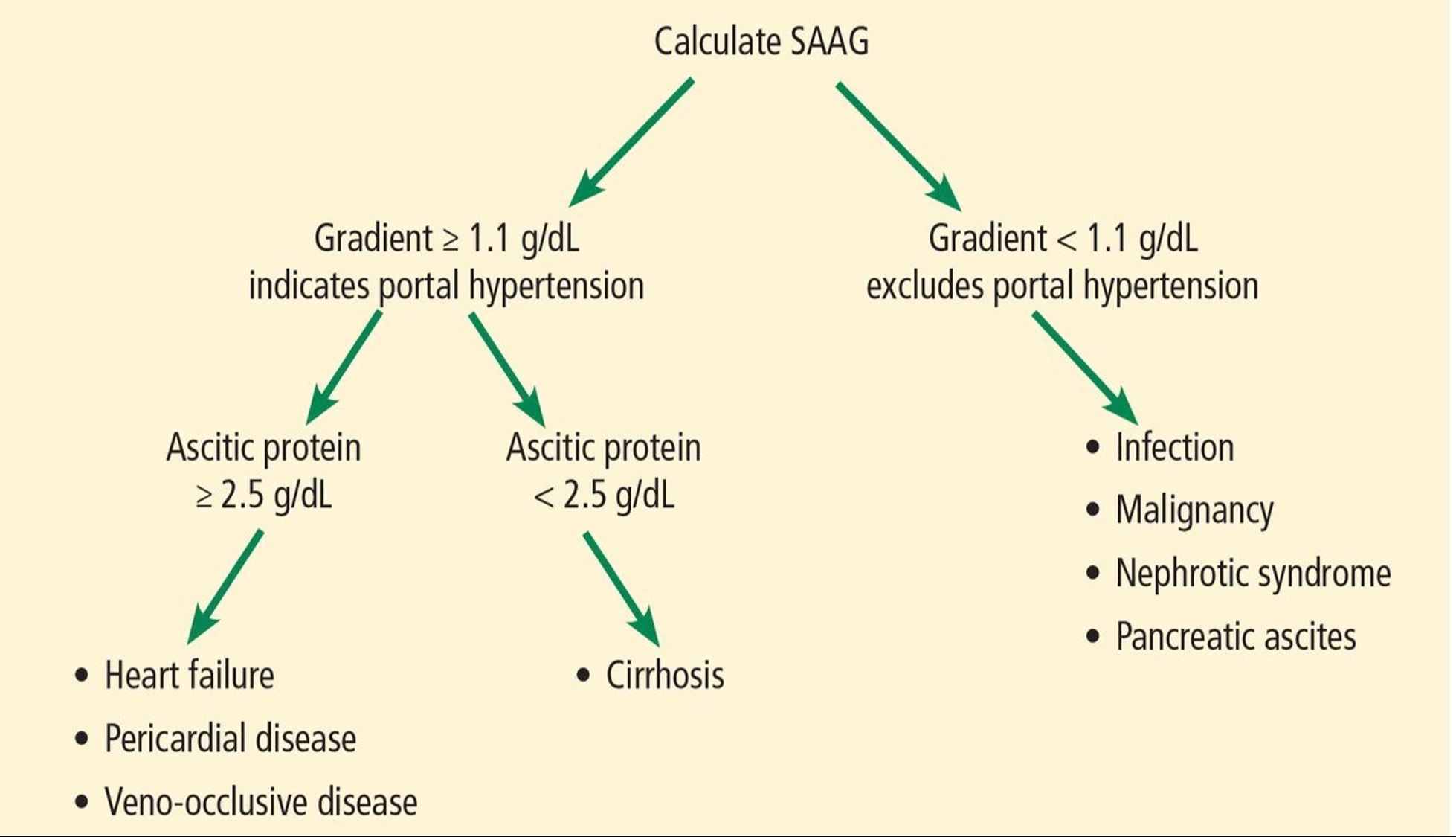
Figure: Figure 1: Workup of abdominal ascites
Disclosures:
Elona Poltiyelova indicated no relevant financial relationships.
Aaron Schluger indicated no relevant financial relationships.
Virendra Tewari indicated no relevant financial relationships.
Elona Poltiyelova, DO, Aaron Schluger, MD, Virendra Tewari, MD, FACG. P3037 - Nephrogenic Ascites: A Rare Cause of Refractory Ascites, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

