Monday Poster Session
Category: Liver
P3044 - Acute Exacerbation of Autoimmune Hepatitis Caused by Localized Cytomegalovirus Reactivation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ES
Elen Sarkisyan, DO
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Elen Sarkisyan, DO, Dai-an Vo-Ba, DO, Arjun Ponduri, MD, Levon Tantoushian, DO, Phillip Oberg, DO, Vishvinder Sharma, MD, Mark Mckenzie, MD
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Autoimmune hepatitis (AIH) is an inflammatory liver disease characterized by elevated immunoglobulins and autoantibodies. The cause of AIH is not fully understood but environmental, genetic and immunologic factors are believed to be contributing factors. Patients may suffer from acute exacerbations of AIH triggered by viral illnesses. Cytomegalovirus (CMV) is a common viral illness that can lead to severe complications in people with autoimmune diseases such as AIH.
We present a 66-year-old female with biopsy-proven AIH on mycophenolate mofetil who presented with 2 weeks of worsening jaundice and was found to have acute-on-chronic hepatitis caused by localized CMV reactivation.
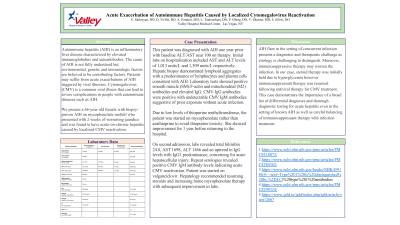
Case Description/Methods: This patient was diagnosed with AIH one year prior with baseline ALT/AST near 100 on therapy. Initial labs on hospitalization included AST and ALT levels of 1,013 units/L and 1,309 units/L respectively. Hepatic biopsy demonstrated lymphoid aggregates with a predominance of lymphocytes and plasma cells consistent with AIH. Laboratory tests showed positive smooth muscle (SM)/F-actin and mitochondrial (M2) antibodies and elevated IgG. CMV IgG antibodies were positive with undetectable CMV IgM antibodies suggestive of prior exposure without acute infection.
Due to low levels of thiopurine methyltransferase, the patient was started on mycophenolate rather than azathioprine to avoid thiopurine toxicity. She showed improvement for 1 year before returning to the hospital.
On second admission, labs revealed total bilirubin 24.8, AST 1698, ALT 1466 and an uptrend in IgG levels with IgG1 predominance, concerning for acute hepatocellular injury. Repeat serologies revealed positive CMV IgM antibody levels indicating acute CMV reactivation. Patient was started on valganciclovir. Hepatology recommended resuming steroids and increasing home mycophenolate therapy with subsequent improvement in labs.
Discussion: AIH flare in the setting of concurrent infection presents a diagnostic and therapeutic challenge as etiology is challenging to distinguish. Moreover, immunosuppressive therapy may worsen the infection. In our case, steroid therapy was initially held due to hyperglycemia however immunosuppressant therapy was resumed following antiviral therapy for CMV treatment. This case demonstrates the importance of a broad list of differential diagnoses and thorough diagnostic testing for acute hepatitis even in the setting of known AIH as well as careful balancing of immunosuppressant therapy with infection treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elen Sarkisyan, DO, Dai-an Vo-Ba, DO, Arjun Ponduri, MD, Levon Tantoushian, DO, Phillip Oberg, DO, Vishvinder Sharma, MD, Mark Mckenzie, MD. P3044 - Acute Exacerbation of Autoimmune Hepatitis Caused by Localized Cytomegalovirus Reactivation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Autoimmune hepatitis (AIH) is an inflammatory liver disease characterized by elevated immunoglobulins and autoantibodies. The cause of AIH is not fully understood but environmental, genetic and immunologic factors are believed to be contributing factors. Patients may suffer from acute exacerbations of AIH triggered by viral illnesses. Cytomegalovirus (CMV) is a common viral illness that can lead to severe complications in people with autoimmune diseases such as AIH.
We present a 66-year-old female with biopsy-proven AIH on mycophenolate mofetil who presented with 2 weeks of worsening jaundice and was found to have acute-on-chronic hepatitis caused by localized CMV reactivation.
Case Description/Methods: This patient was diagnosed with AIH one year prior with baseline ALT/AST near 100 on therapy. Initial labs on hospitalization included AST and ALT levels of 1,013 units/L and 1,309 units/L respectively. Hepatic biopsy demonstrated lymphoid aggregates with a predominance of lymphocytes and plasma cells consistent with AIH. Laboratory tests showed positive smooth muscle (SM)/F-actin and mitochondrial (M2) antibodies and elevated IgG. CMV IgG antibodies were positive with undetectable CMV IgM antibodies suggestive of prior exposure without acute infection.
Due to low levels of thiopurine methyltransferase, the patient was started on mycophenolate rather than azathioprine to avoid thiopurine toxicity. She showed improvement for 1 year before returning to the hospital.
On second admission, labs revealed total bilirubin 24.8, AST 1698, ALT 1466 and an uptrend in IgG levels with IgG1 predominance, concerning for acute hepatocellular injury. Repeat serologies revealed positive CMV IgM antibody levels indicating acute CMV reactivation. Patient was started on valganciclovir. Hepatology recommended resuming steroids and increasing home mycophenolate therapy with subsequent improvement in labs.
Discussion: AIH flare in the setting of concurrent infection presents a diagnostic and therapeutic challenge as etiology is challenging to distinguish. Moreover, immunosuppressive therapy may worsen the infection. In our case, steroid therapy was initially held due to hyperglycemia however immunosuppressant therapy was resumed following antiviral therapy for CMV treatment. This case demonstrates the importance of a broad list of differential diagnoses and thorough diagnostic testing for acute hepatitis even in the setting of known AIH as well as careful balancing of immunosuppressant therapy with infection treatment.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Elen Sarkisyan indicated no relevant financial relationships.
Dai-an Vo-Ba indicated no relevant financial relationships.
Arjun Ponduri indicated no relevant financial relationships.
Levon Tantoushian indicated no relevant financial relationships.
Phillip Oberg indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Mark Mckenzie indicated no relevant financial relationships.
Elen Sarkisyan, DO, Dai-an Vo-Ba, DO, Arjun Ponduri, MD, Levon Tantoushian, DO, Phillip Oberg, DO, Vishvinder Sharma, MD, Mark Mckenzie, MD. P3044 - Acute Exacerbation of Autoimmune Hepatitis Caused by Localized Cytomegalovirus Reactivation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
