Monday Poster Session
Category: Liver
P3045 - Complexities of Managing Chronic Hepatitis B in HIV: A Case of Acute Liver Injury Post-Medication Change
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Manasa Ginjupalli, MBBS, MD
The Brooklyn Hospital Center
New York, NY
Presenting Author(s)
Manasa Ginjupalli, MBBS, MD1, Hamsika Moparty, MD2, Jayalekshmi Jayakumar, MBBS, MD2, Sweta Lohani, MBBS, MD3, Nishanth Moparty, MBBS4, Hima Varsha. Voruganti, MBBS, MD5, Ishwari Iyer, MBBS, MD3, Rishav Sinha, MD3, Camelia Ciobanu, MD3, Arnold N. Forlemu, MD, MPH6, Ali Wakil, MD3, Praneeth Bandaru, MBBS, MD3, Mohammad Nawaz, MD3
1The Brooklyn Hospital Center, New York, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Brooklyn Hospital Center, Brooklyn, NY; 4Bhaskar Medical College, Hyderabad, Telangana, India; 5North Alabama Medical Center, Florence, AL; 6Brooklyn Hospital Center, Athens, GA
Introduction: Chronic hepatitis B is an indolent condition which occurs as a consequence of persistent infection with hepatitis B virus (HBV). Acute flare ups and presence of high viral loads are considered indications for initiating treatment. Co-infection of HBV with HIV and other viruses are not uncommon and could lead to an array of complications as a result of infection, treatment alteration and disease progression. We present the case of a chronic hepatitis B carrier with well-controlled HIV infection, who subsequently developed acute liver injury secondary to HBV flareup, following alterations in her HIV treatment regimen, notably after discontinuation of Tenofovir.
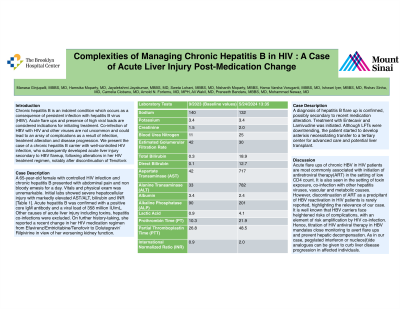
Case Description/Methods: A 65-year-old female with controlled HIV infection and chronic hepatitis B presented with abdominal pain and non bloody emesis for a day. Vitals and physical exam was unremarkable. Initial labs showed severe hepatocellular injury with markedly elevated AST/ALT, bilirubin and INR [Table 1]. Acute hepatitis B was confirmed with a positive core IgM antibody and a viral load of 358 million IU/mL. Other causes of acute liver injury including toxins, hepatitis coinfections were excluded. On further history-taking, she reported a recent change in her HIV medication regimen from Efavirenz/Emtricitabine/Tenofovir to Dolutegravir/Rilpivirine in view of her worsening kidney function. A diagnosis of hepatitis B flare up is confirmed, possibly secondary to recent medication alteration. Treatment with Entecavir and Lamivudine was initiated. Although LFTs were downtrending, the patient started to develop asterixis necessitating transfer to a tertiary center for advanced care and potential liver transplant.
Discussion: Acute flare ups of chronic HBV in HIV patients are most commonly associated with initiation of antiretroviral therapy(ART) in the setting of low CD4 count. It is also seen in the setting of toxin exposure, co-infection with other hepatitis viruses, vascular and metabolic causes. However, discontinuation of ART as a precipitant of HBV reactivation in HIV patients is rarely reported, highlighting the relevance of our case. It is well known that HBV carriers face heightened risks of complications, with an element of risk amplification by HIV co-infection. Hence, titration of HIV antiviral therapy in HBV mandates close monitoring to avert flare ups and prevent hepatic decompensation. As in our case, pegylated interferon or nucleos(t)ide analogues can be given to curb liver disease progression in affected individuals.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Manasa Ginjupalli, MBBS, MD1, Hamsika Moparty, MD2, Jayalekshmi Jayakumar, MBBS, MD2, Sweta Lohani, MBBS, MD3, Nishanth Moparty, MBBS4, Hima Varsha. Voruganti, MBBS, MD5, Ishwari Iyer, MBBS, MD3, Rishav Sinha, MD3, Camelia Ciobanu, MD3, Arnold N. Forlemu, MD, MPH6, Ali Wakil, MD3, Praneeth Bandaru, MBBS, MD3, Mohammad Nawaz, MD3. P3045 - Complexities of Managing Chronic Hepatitis B in HIV: A Case of Acute Liver Injury Post-Medication Change, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The Brooklyn Hospital Center, New York, NY; 2The Brooklyn Hospital Center, Brooklyn, NY; 3Brooklyn Hospital Center, Brooklyn, NY; 4Bhaskar Medical College, Hyderabad, Telangana, India; 5North Alabama Medical Center, Florence, AL; 6Brooklyn Hospital Center, Athens, GA
Introduction: Chronic hepatitis B is an indolent condition which occurs as a consequence of persistent infection with hepatitis B virus (HBV). Acute flare ups and presence of high viral loads are considered indications for initiating treatment. Co-infection of HBV with HIV and other viruses are not uncommon and could lead to an array of complications as a result of infection, treatment alteration and disease progression. We present the case of a chronic hepatitis B carrier with well-controlled HIV infection, who subsequently developed acute liver injury secondary to HBV flareup, following alterations in her HIV treatment regimen, notably after discontinuation of Tenofovir.
Case Description/Methods: A 65-year-old female with controlled HIV infection and chronic hepatitis B presented with abdominal pain and non bloody emesis for a day. Vitals and physical exam was unremarkable. Initial labs showed severe hepatocellular injury with markedly elevated AST/ALT, bilirubin and INR [Table 1]. Acute hepatitis B was confirmed with a positive core IgM antibody and a viral load of 358 million IU/mL. Other causes of acute liver injury including toxins, hepatitis coinfections were excluded. On further history-taking, she reported a recent change in her HIV medication regimen from Efavirenz/Emtricitabine/Tenofovir to Dolutegravir/Rilpivirine in view of her worsening kidney function. A diagnosis of hepatitis B flare up is confirmed, possibly secondary to recent medication alteration. Treatment with Entecavir and Lamivudine was initiated. Although LFTs were downtrending, the patient started to develop asterixis necessitating transfer to a tertiary center for advanced care and potential liver transplant.
Discussion: Acute flare ups of chronic HBV in HIV patients are most commonly associated with initiation of antiretroviral therapy(ART) in the setting of low CD4 count. It is also seen in the setting of toxin exposure, co-infection with other hepatitis viruses, vascular and metabolic causes. However, discontinuation of ART as a precipitant of HBV reactivation in HIV patients is rarely reported, highlighting the relevance of our case. It is well known that HBV carriers face heightened risks of complications, with an element of risk amplification by HIV co-infection. Hence, titration of HIV antiviral therapy in HBV mandates close monitoring to avert flare ups and prevent hepatic decompensation. As in our case, pegylated interferon or nucleos(t)ide analogues can be given to curb liver disease progression in affected individuals.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Manasa Ginjupalli indicated no relevant financial relationships.
Hamsika Moparty indicated no relevant financial relationships.
Jayalekshmi Jayakumar indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Nishanth Moparty indicated no relevant financial relationships.
Hima Voruganti indicated no relevant financial relationships.
Ishwari Iyer indicated no relevant financial relationships.
Rishav Sinha indicated no relevant financial relationships.
Camelia Ciobanu indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Mohammad Nawaz indicated no relevant financial relationships.
Manasa Ginjupalli, MBBS, MD1, Hamsika Moparty, MD2, Jayalekshmi Jayakumar, MBBS, MD2, Sweta Lohani, MBBS, MD3, Nishanth Moparty, MBBS4, Hima Varsha. Voruganti, MBBS, MD5, Ishwari Iyer, MBBS, MD3, Rishav Sinha, MD3, Camelia Ciobanu, MD3, Arnold N. Forlemu, MD, MPH6, Ali Wakil, MD3, Praneeth Bandaru, MBBS, MD3, Mohammad Nawaz, MD3. P3045 - Complexities of Managing Chronic Hepatitis B in HIV: A Case of Acute Liver Injury Post-Medication Change, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
