Monday Poster Session
Category: Liver
P3050 - Acute Fulminant Hepatitis Induced by Bacillus cereus: A Case Study and Clinical Insights
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Warsha Mal Korani, MBBS
Conemaugh Memorial Medical Center
JOHNSTOWN, PA
Presenting Author(s)
Warsha Mal Korani, MBBS1, Rishi Chowdhary, MBBS2, Adel Farhoud, MD3
1Conemaugh Memorial Medical Center, Johnstown, PA; 2Case Western Reserve University, Cleveland, OH; 3Lahey Hospital and Medical Center, Manchester, NH
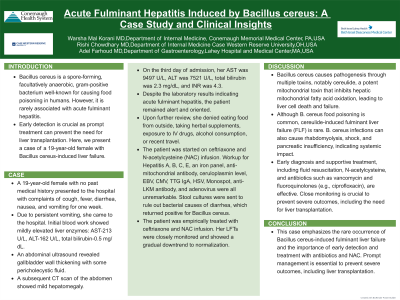
Introduction: Bacillus cereus is a spore-forming, facultatively anaerobic, gram-positive bacterium well-known for causing food poisoning in humans. However, it is rarely associated with acute fulminant hepatitis. Early detection is crucial as prompt treatment can prevent the need for liver transplantation. Here, we present a case of a 19-year-old female with Bacillus cereus-induced liver failure.
Case Description/Methods: A 19-year-old female with no past medical history presented to the hospital with complaints of cough, fever, diarrhea, nausea, and vomiting for one week. Due to persistent vomiting, she came to the hospital. Initial blood work showed mildly elevated liver enzymes: AST-213 U/L, ALT-162 U/L, total bilirubin-0.5 mg/dL,. An abdominal ultrasound revealed gallbladder wall thickening with some pericholecystic fluid. A subsequent CT scan of the abdomen showed mild hepatomegaly.On the third day of admission, her AST was 9497 U/L, ALT was 7521 U/L, total bilirubin was 2.3 mg/dL, and INR was 4.3. Despite the laboratory results indicating acute fulminant hepatitis, the patient remained alert and oriented. Upon further review, she denied eating food from outside, taking herbal supplements, exposure to IV drugs, alcohol consumption, or recent travel.The patient was started on ceftriaxone and N-acetylcysteine (NAC) infusion. Workup for Hepatitis A, B, C, E, an iron panel, anti-mitochondrial antibody, ceruloplasmin level, EBV, CMV, TTG IgA, HSV, Monospot, anti-LKM antibody, and adenovirus were all unremarkable. Stool cultures were sent to rule out bacterial causes of diarrhea, which returned positive for Bacillus cereus.The patient was empirically treated with ceftriaxone and NAC infusion. Her LFTs were closely monitored and showed a gradual downtrend to normalization.
Discussion: Bacillus cereus causes pathogenesis through multiple toxins, notably cereulide, a potent mitochondrial toxin that inhibits hepatic mitochondrial fatty acid oxidation, leading to liver cell death and failure. Although B. cereus food poisoning is common, cereulide-induced fulminant liver failure (FLF) is rare. B. cereus infections can also cause rhabdomyolysis, shock, and pancreatic insufficiency, indicating systemic impact. Early diagnosis and supportive treatment, including fluid resuscitation, N-acetylcysteine, and antibiotics such as vancomycin and fluoroquinolones (e.g., ciprofloxacin), are effective. Close monitoring is crucial to prevent severe outcomes, including the need for liver transplantation.
Disclosures:
Warsha Mal Korani, MBBS1, Rishi Chowdhary, MBBS2, Adel Farhoud, MD3. P3050 - Acute Fulminant Hepatitis Induced by <i>Bacillus cereus</i>: A Case Study and Clinical Insights, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Conemaugh Memorial Medical Center, Johnstown, PA; 2Case Western Reserve University, Cleveland, OH; 3Lahey Hospital and Medical Center, Manchester, NH
Introduction: Bacillus cereus is a spore-forming, facultatively anaerobic, gram-positive bacterium well-known for causing food poisoning in humans. However, it is rarely associated with acute fulminant hepatitis. Early detection is crucial as prompt treatment can prevent the need for liver transplantation. Here, we present a case of a 19-year-old female with Bacillus cereus-induced liver failure.
Case Description/Methods: A 19-year-old female with no past medical history presented to the hospital with complaints of cough, fever, diarrhea, nausea, and vomiting for one week. Due to persistent vomiting, she came to the hospital. Initial blood work showed mildly elevated liver enzymes: AST-213 U/L, ALT-162 U/L, total bilirubin-0.5 mg/dL,. An abdominal ultrasound revealed gallbladder wall thickening with some pericholecystic fluid. A subsequent CT scan of the abdomen showed mild hepatomegaly.On the third day of admission, her AST was 9497 U/L, ALT was 7521 U/L, total bilirubin was 2.3 mg/dL, and INR was 4.3. Despite the laboratory results indicating acute fulminant hepatitis, the patient remained alert and oriented. Upon further review, she denied eating food from outside, taking herbal supplements, exposure to IV drugs, alcohol consumption, or recent travel.The patient was started on ceftriaxone and N-acetylcysteine (NAC) infusion. Workup for Hepatitis A, B, C, E, an iron panel, anti-mitochondrial antibody, ceruloplasmin level, EBV, CMV, TTG IgA, HSV, Monospot, anti-LKM antibody, and adenovirus were all unremarkable. Stool cultures were sent to rule out bacterial causes of diarrhea, which returned positive for Bacillus cereus.The patient was empirically treated with ceftriaxone and NAC infusion. Her LFTs were closely monitored and showed a gradual downtrend to normalization.
Discussion: Bacillus cereus causes pathogenesis through multiple toxins, notably cereulide, a potent mitochondrial toxin that inhibits hepatic mitochondrial fatty acid oxidation, leading to liver cell death and failure. Although B. cereus food poisoning is common, cereulide-induced fulminant liver failure (FLF) is rare. B. cereus infections can also cause rhabdomyolysis, shock, and pancreatic insufficiency, indicating systemic impact. Early diagnosis and supportive treatment, including fluid resuscitation, N-acetylcysteine, and antibiotics such as vancomycin and fluoroquinolones (e.g., ciprofloxacin), are effective. Close monitoring is crucial to prevent severe outcomes, including the need for liver transplantation.
Disclosures:
Warsha Mal Korani indicated no relevant financial relationships.
Rishi Chowdhary indicated no relevant financial relationships.
Adel Farhoud indicated no relevant financial relationships.
Warsha Mal Korani, MBBS1, Rishi Chowdhary, MBBS2, Adel Farhoud, MD3. P3050 - Acute Fulminant Hepatitis Induced by <i>Bacillus cereus</i>: A Case Study and Clinical Insights, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
