Monday Poster Session
Category: Liver
P3055 - A Rare Case of Seronegative Autoimmune Hepatitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Bharati Dev, DO
Icahn School of Medicine at Mount Sinai Morningside/West
New York, NY
Presenting Author(s)
Bharati Dev, DO1, Jake DeBroff, MD2, Mako Koseki, MD2, Liliana Vittini-Hernandez, MD2, Piya Kositangool, MD2, Kevin Jordan, MD2
1Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY; 2Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Autoimmune hepatitis (AIH) is an inflammatory disease with an incidence of 0.7 to 2 per 100,000 population. Diagnosis is clinically made with symptoms and elevated globulins and serological markers. Liver biopsy is considered when serology is negative. We present a case of seronegative AIH in the setting of negative viral, metabolic, and autoimmune workup.
Case Description/Methods: A 37-year-old male with no medical history presented with 6 days of generalized fatigue and elevated liver function tests (LFTs). Associated symptoms included vomiting, jaundice, and epigastric discomfort. The patient denied family history of GI malignancy, autoimmune disease, hepatitis history, recent travel, or use of substances, alcohol, supplements, and over the counter medications.
Initial labs showed an aspartate aminotransferase of 1055 U/L, alanine transaminase of 2056 U/L, total bilirubin of 6.7mg/dL, direct bilirubin of 5.0mg/dL, and ferritin of 4313ug/L. Urine toxicology was normal. Viral hepatitis panel revealed immunity from vaccines. Serum immunoglobulins, toxin and autoimmune antibody levels were normal. Inflammatory markers of C-reactive protein and lactate dehydrogenase were elevated. Ceruloplasmin and alpha-1 antitrypsin were increased, ruling out genetic causes. Both abdominal ultrasound and MRCP showed hepatic steatosis.
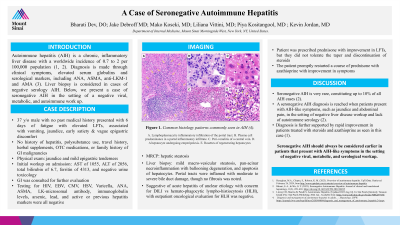
Liver biopsy revealed macrovesicular steatosis, panacinar inflammation and hepatocyte apoptosis. Portal tracts had moderate to severe ductal damage with no fibrosis. These findings suggested acute hepatitis of unclear etiology with concern for drug-induced liver injury versus hemophagocytic lymphohistiocytosis (HLH). However, oncological evaluation for HLH was negative. Workup was otherwise negative and the patient began a steroid course for suspected autoimmune hepatitis with improvement in LFTs.
The patient, however, did not tolerate the tapered discontinuation of steroids, as symptoms reoccurred. Prednisone and azathioprine were promptly restarted with improvement in symptoms and bloodwork.
Discussion: Seronegative AIH is very rare, constituting up to 10% of AIH cases. Seronegative AIH is determined when patients present with AIH-like symptoms in the setting of negative workup and lack of elevated globulins or serology. This diagnosis is further supported through rapid clinical improvement with steroids and azathioprine, as noted above. Seronegative AIH should be considered in patients with AIH-like symptoms in the setting of negative viral, metabolic, and serological workup.
Disclosures:
Bharati Dev, DO1, Jake DeBroff, MD2, Mako Koseki, MD2, Liliana Vittini-Hernandez, MD2, Piya Kositangool, MD2, Kevin Jordan, MD2. P3055 - A Rare Case of Seronegative Autoimmune Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY; 2Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Autoimmune hepatitis (AIH) is an inflammatory disease with an incidence of 0.7 to 2 per 100,000 population. Diagnosis is clinically made with symptoms and elevated globulins and serological markers. Liver biopsy is considered when serology is negative. We present a case of seronegative AIH in the setting of negative viral, metabolic, and autoimmune workup.
Case Description/Methods: A 37-year-old male with no medical history presented with 6 days of generalized fatigue and elevated liver function tests (LFTs). Associated symptoms included vomiting, jaundice, and epigastric discomfort. The patient denied family history of GI malignancy, autoimmune disease, hepatitis history, recent travel, or use of substances, alcohol, supplements, and over the counter medications.
Initial labs showed an aspartate aminotransferase of 1055 U/L, alanine transaminase of 2056 U/L, total bilirubin of 6.7mg/dL, direct bilirubin of 5.0mg/dL, and ferritin of 4313ug/L. Urine toxicology was normal. Viral hepatitis panel revealed immunity from vaccines. Serum immunoglobulins, toxin and autoimmune antibody levels were normal. Inflammatory markers of C-reactive protein and lactate dehydrogenase were elevated. Ceruloplasmin and alpha-1 antitrypsin were increased, ruling out genetic causes. Both abdominal ultrasound and MRCP showed hepatic steatosis.
Liver biopsy revealed macrovesicular steatosis, panacinar inflammation and hepatocyte apoptosis. Portal tracts had moderate to severe ductal damage with no fibrosis. These findings suggested acute hepatitis of unclear etiology with concern for drug-induced liver injury versus hemophagocytic lymphohistiocytosis (HLH). However, oncological evaluation for HLH was negative. Workup was otherwise negative and the patient began a steroid course for suspected autoimmune hepatitis with improvement in LFTs.
The patient, however, did not tolerate the tapered discontinuation of steroids, as symptoms reoccurred. Prednisone and azathioprine were promptly restarted with improvement in symptoms and bloodwork.
Discussion: Seronegative AIH is very rare, constituting up to 10% of AIH cases. Seronegative AIH is determined when patients present with AIH-like symptoms in the setting of negative workup and lack of elevated globulins or serology. This diagnosis is further supported through rapid clinical improvement with steroids and azathioprine, as noted above. Seronegative AIH should be considered in patients with AIH-like symptoms in the setting of negative viral, metabolic, and serological workup.
Disclosures:
Bharati Dev indicated no relevant financial relationships.
Jake DeBroff indicated no relevant financial relationships.
Mako Koseki indicated no relevant financial relationships.
Liliana Vittini-Hernandez indicated no relevant financial relationships.
Piya Kositangool indicated no relevant financial relationships.
Kevin Jordan indicated no relevant financial relationships.
Bharati Dev, DO1, Jake DeBroff, MD2, Mako Koseki, MD2, Liliana Vittini-Hernandez, MD2, Piya Kositangool, MD2, Kevin Jordan, MD2. P3055 - A Rare Case of Seronegative Autoimmune Hepatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
