Monday Poster Session
Category: Liver
P3060 - Acquired Gilbert’s Secondary to Liver Transplant in Pre-Transplant Gilbert-Negative Patient Sparked by COVID-19 Vaccination
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Raza Muhammad, DO
University of Chicago Northshore
Chicago, IL
Presenting Author(s)
Raza Muhammad, DO1, Edward Villa, MD2, Mitchelle V. Zolotarevsky, MD3
1University of Chicago Northshore, Evanston, IL; 2NorthShore University HealthSystem, Evanston, IL; 3University of Chicago, NorthShore Internal Medicine, Chicago, IL
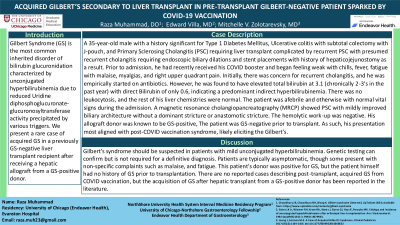
Introduction: Gilbert Syndrome (GS) is the most common inherited disorder of bilirubin glucuronidation characterized by unconjugated hyperbilirubinemia due to reduced Uridine diphosphoglucuronate-glucuronosyltransferase activity precipitated by various triggers. We present a rare case of acquired GS in a previously GS-negative liver transplant recipient after receiving a hepatic allograft from a GS-positive donor.
Case Description/Methods: 35-year-old male with history significant for Type 1 Diabetes Mellitus, Ulcerative colitis with subtotal colectomy with J-pouch and Primary Sclerosing Cholangitis (PSC) requiring liver transplant complicated by recurrent PSC with presumed recurrent cholangitis requiring endoscopic biliary dilations and stent placements with history of hepaticojejunostomy as a result. Prior to admission, he had recently received his COVID booster and began feeling weak with chills, fever, fatigue with malaise, myalgias, and right upper quadrant pain. Initially, there was concern for recurrent cholangitis, and he was empirically started on antibiotics. However, he was found to have elevated total bilirubin at 3.1 (chronically 2-3's in the past year) with direct Bilirubin of only 0.6, indicating a predominant indirect hyperbilirubinemia. There was no leukocytosis, and the rest of his liver chemistries were normal. Patient was afebrile and otherwise with normal vital signs during the admission. A magnetic resonance cholangiopancreatography (MRCP) showed known PSC with mildly improved biliary architecture without a dominant stricture or anastomotic stricture. The hemolytic work-up was negative. His allograft donor was known to be GS-positive, the patient was GS-negative prior to transplant. As such, his presentation most aligned with post-COVID vaccination syndrome, likely eliciting the Gilbert’s.
Discussion: Gilbert’s syndrome should be suspected in patients with mild unconjugated hyperbilirubinemia. Genetic testing can confirm but is not required for a definitive diagnosis. Patients are typically asymptomatic, though some present with non-specific complaints such as malaise, and fatigue. This patient's donor was positive for GS, but the patient himself had no history of GS prior to transplantation. There are no reported cases describing post-transplant, acquired GS from COVID vaccination, but acquisition of GS after hepatic transplant from a GS-positive donor has been reported in the literature.
Disclosures:
Raza Muhammad, DO1, Edward Villa, MD2, Mitchelle V. Zolotarevsky, MD3. P3060 - Acquired Gilbert’s Secondary to Liver Transplant in Pre-Transplant Gilbert-Negative Patient Sparked by COVID-19 Vaccination, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Chicago Northshore, Evanston, IL; 2NorthShore University HealthSystem, Evanston, IL; 3University of Chicago, NorthShore Internal Medicine, Chicago, IL
Introduction: Gilbert Syndrome (GS) is the most common inherited disorder of bilirubin glucuronidation characterized by unconjugated hyperbilirubinemia due to reduced Uridine diphosphoglucuronate-glucuronosyltransferase activity precipitated by various triggers. We present a rare case of acquired GS in a previously GS-negative liver transplant recipient after receiving a hepatic allograft from a GS-positive donor.
Case Description/Methods: 35-year-old male with history significant for Type 1 Diabetes Mellitus, Ulcerative colitis with subtotal colectomy with J-pouch and Primary Sclerosing Cholangitis (PSC) requiring liver transplant complicated by recurrent PSC with presumed recurrent cholangitis requiring endoscopic biliary dilations and stent placements with history of hepaticojejunostomy as a result. Prior to admission, he had recently received his COVID booster and began feeling weak with chills, fever, fatigue with malaise, myalgias, and right upper quadrant pain. Initially, there was concern for recurrent cholangitis, and he was empirically started on antibiotics. However, he was found to have elevated total bilirubin at 3.1 (chronically 2-3's in the past year) with direct Bilirubin of only 0.6, indicating a predominant indirect hyperbilirubinemia. There was no leukocytosis, and the rest of his liver chemistries were normal. Patient was afebrile and otherwise with normal vital signs during the admission. A magnetic resonance cholangiopancreatography (MRCP) showed known PSC with mildly improved biliary architecture without a dominant stricture or anastomotic stricture. The hemolytic work-up was negative. His allograft donor was known to be GS-positive, the patient was GS-negative prior to transplant. As such, his presentation most aligned with post-COVID vaccination syndrome, likely eliciting the Gilbert’s.
Discussion: Gilbert’s syndrome should be suspected in patients with mild unconjugated hyperbilirubinemia. Genetic testing can confirm but is not required for a definitive diagnosis. Patients are typically asymptomatic, though some present with non-specific complaints such as malaise, and fatigue. This patient's donor was positive for GS, but the patient himself had no history of GS prior to transplantation. There are no reported cases describing post-transplant, acquired GS from COVID vaccination, but acquisition of GS after hepatic transplant from a GS-positive donor has been reported in the literature.
Disclosures:
Raza Muhammad indicated no relevant financial relationships.
Edward Villa: Interscope – Consultant. Olympus Corp – Consultant.
Mitchelle Zolotarevsky indicated no relevant financial relationships.
Raza Muhammad, DO1, Edward Villa, MD2, Mitchelle V. Zolotarevsky, MD3. P3060 - Acquired Gilbert’s Secondary to Liver Transplant in Pre-Transplant Gilbert-Negative Patient Sparked by COVID-19 Vaccination, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
