Monday Poster Session
Category: Liver
P3063 - A Case of Esophageal Variceal Hemorrhage With Normal Portal Pressures: Lessons From the Baveno VII Consensus on Porto-Sinusoidal Vascular Disorder
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Akash Keluth Chavan, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Akash Keluth Chavan, MD, Michael Saadeh, MD, Sofi Damjanovska, MD, Naemat Sandhu, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
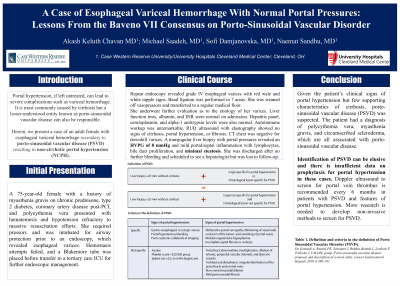
Introduction: Cirrhosis is the most common etiology for portal hypertension. A lesser-known entity is porto-sinusoidal vascular disease (PSVD). Herein, we present a case of an adult woman with esophageal variceal hemorrhage secondary to porto-sinusoidal vascular disease (PSVD), resulting in non-cirrhotic portal hypertension.
Case Description/Methods: A 75-year-old woman with a history of myasthenia gravis on chronic prednisone, type 2 diabetes, coronary artery disease post-percutaneous coronary intervention, scleroderma, and polycythemia vera, presented with hematemesis leading to hemorrhagic shock. Endoscopy revealed esophageal varices but hemostasis attempts failed. A Blakemore tube was placed before transfer to our tertiary care medical intensive care unit for further endoscopic management.
Repeat endoscopy revealed grade III esophageal varices with red wale and white nipple signs. Successful band ligation was performed in 7 areas. She was weaned off vasopressors and transferred to a general medicine floor. She underwent further evaluation to assess the etiology for varices. Liver function tests, albumin, and INR were normal on admission. Viral hepatitis panel, ceruloplasmin, smooth muscle antibodies, antibodies to liver-kidney microsome, and alpha-1 antitrypsin levels were unremarkable. Right upper quadrant ultrasound with doppler did not reveal a thrombus in the portal system and ultrasound with elastography staged the fibrosis as F0 based on a stiffness of 4.46 kPA, although there was significant variability. The CT chest was negative for downhill varices. A transjugular liver biopsy with portal pressure measurement revealed bridging fibrosis with minimal steatosis and a hepatic venous pressure gradient (HVPG) of 8 mmHg. She was discharged given no further bleeding and scheduled to see a hepatologist but was lost to follow-up.
Discussion: Identification of PSVD can be elusive and there is insufficient data on the preferred prophylaxis for portal hypertension in these cases. Currently, management is based on cirrhosis guidelines. In patients with clinical signs of portal hypertension but with HVPG< 10 mm hg, PSVD must be ruled out. Given the patient’s clinical signs of portal hypertension and the exclusion of cirrhosis and of other causes of portal hypertension, PSVD can be diagnosed. The patient also had a diagnosis of polycythemia vera, myasthenia gravis, and scleroderma, which are all associated with PSVD.
Disclosures:
Akash Keluth Chavan, MD, Michael Saadeh, MD, Sofi Damjanovska, MD, Naemat Sandhu, MD. P3063 - A Case of Esophageal Variceal Hemorrhage With Normal Portal Pressures: Lessons From the Baveno VII Consensus on Porto-Sinusoidal Vascular Disorder, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH
Introduction: Cirrhosis is the most common etiology for portal hypertension. A lesser-known entity is porto-sinusoidal vascular disease (PSVD). Herein, we present a case of an adult woman with esophageal variceal hemorrhage secondary to porto-sinusoidal vascular disease (PSVD), resulting in non-cirrhotic portal hypertension.
Case Description/Methods: A 75-year-old woman with a history of myasthenia gravis on chronic prednisone, type 2 diabetes, coronary artery disease post-percutaneous coronary intervention, scleroderma, and polycythemia vera, presented with hematemesis leading to hemorrhagic shock. Endoscopy revealed esophageal varices but hemostasis attempts failed. A Blakemore tube was placed before transfer to our tertiary care medical intensive care unit for further endoscopic management.
Repeat endoscopy revealed grade III esophageal varices with red wale and white nipple signs. Successful band ligation was performed in 7 areas. She was weaned off vasopressors and transferred to a general medicine floor. She underwent further evaluation to assess the etiology for varices. Liver function tests, albumin, and INR were normal on admission. Viral hepatitis panel, ceruloplasmin, smooth muscle antibodies, antibodies to liver-kidney microsome, and alpha-1 antitrypsin levels were unremarkable. Right upper quadrant ultrasound with doppler did not reveal a thrombus in the portal system and ultrasound with elastography staged the fibrosis as F0 based on a stiffness of 4.46 kPA, although there was significant variability. The CT chest was negative for downhill varices. A transjugular liver biopsy with portal pressure measurement revealed bridging fibrosis with minimal steatosis and a hepatic venous pressure gradient (HVPG) of 8 mmHg. She was discharged given no further bleeding and scheduled to see a hepatologist but was lost to follow-up.
Discussion: Identification of PSVD can be elusive and there is insufficient data on the preferred prophylaxis for portal hypertension in these cases. Currently, management is based on cirrhosis guidelines. In patients with clinical signs of portal hypertension but with HVPG< 10 mm hg, PSVD must be ruled out. Given the patient’s clinical signs of portal hypertension and the exclusion of cirrhosis and of other causes of portal hypertension, PSVD can be diagnosed. The patient also had a diagnosis of polycythemia vera, myasthenia gravis, and scleroderma, which are all associated with PSVD.
Disclosures:
Akash Keluth Chavan indicated no relevant financial relationships.
Michael Saadeh indicated no relevant financial relationships.
Sofi Damjanovska indicated no relevant financial relationships.
Naemat Sandhu indicated no relevant financial relationships.
Akash Keluth Chavan, MD, Michael Saadeh, MD, Sofi Damjanovska, MD, Naemat Sandhu, MD. P3063 - A Case of Esophageal Variceal Hemorrhage With Normal Portal Pressures: Lessons From the Baveno VII Consensus on Porto-Sinusoidal Vascular Disorder, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
