Monday Poster Session
Category: Liver
P3066 - Pregnancy Under Pressure: Addressing Variceal Bleeding During Gestation
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MM
Momin Masroor, MD
University of California, Irvine
Orange, CA
Presenting Author(s)
Momin Masroor, MD1, Sophie Trujillo, DO2, Erica Duh, MD3, Christina Ling, MD1, Simon Long, MD4, Usman Rahim, MD5, Jason Samarasena, MD1
1University of California, Irvine, Orange, CA; 2University of California Irvine, Irvine, CA; 3University of California Irvine Digestive Health Institute, Orange, CA; 4University of California Irvine Health, Orange, CA; 5University of California Irvine Digestive Health Institute, Exeter, CA
Introduction: Cirrhosis may lead to portal hypertension, which increases the risk of complications such as variceal bleeding. Pregnancy is a condition that is also associated with portal hypertension, as physiological hemodynamic changes worsen portal pressures and increase the risk of variceal bleed. In cirrhotic patients who are pregnant, it is imperative to monitor these patients closely and use a careful interdisciplinary approach. Here we describe the case of a pregnant female with variceal bleeding.
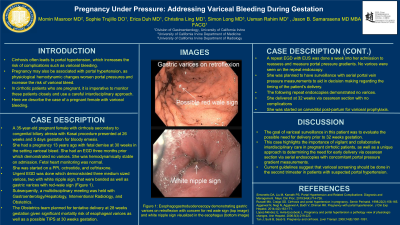
Case Description/Methods: A 35-year-old pregnant female with cirrhosis secondary to congenital biliary atresia with Kasai procedure presented at 26 weeks and 5 days gestation for bloody emesis. She had a prior pregnancy 13 years ago with fetal demise at 30 weeks in the setting variceal bleed. She had an EGD three months prior which demonstrated no varices. She was hemodynamically stable on admission. Fetal heart monitoring was normal. She was started on a PPI, octreotide, and ceftriaxone. Urgent EGD was done which demonstrated three medium sized varices, two with white nipple sign, that were banded as well as gastric varices with red-wale sign. Subsequently, a multidisciplinary meeting was held with Gastroenterology/Hepatology, Interventional Radiology, and Obstetrics. The Obstetrics team planned for tentative delivery at 28 weeks gestation given significant mortality risk of esophageal varices as well as a possible TIPS at 30 weeks gestation. A repeat EGD with EUS was done a week into her admission to reassess and measure portal pressure gradients. No varices were seen on the repeat endoscopy. Given these findings, the plan shifted to weekly EGD surveillance with portal vein pressure measurements to aid in decision making regarding the timing of the patient’s delivery. The following repeat endoscopies demonstrated no varices. She delivered at 32 weeks via cesarean section with no complications and was started on carvedilol for variceal prophylaxis.
Discussion: The goal of variceal surveillance in this patient was to evaluate the possible need for delivery prior to 32 weeks gestation. This case highlights the importance of vigilant and collaborative interdisciplinary care in pregnant cirrhotic patients, as well as a unique approach to determining the need for early delivery via cesarean section via serial endoscopies with concomitant portal pressure gradient measurements. Current guidelines suggest that variceal screening should be done in the second trimester in patients with suspected portal hypertension.
Disclosures:
Momin Masroor, MD1, Sophie Trujillo, DO2, Erica Duh, MD3, Christina Ling, MD1, Simon Long, MD4, Usman Rahim, MD5, Jason Samarasena, MD1. P3066 - Pregnancy Under Pressure: Addressing Variceal Bleeding During Gestation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of California, Irvine, Orange, CA; 2University of California Irvine, Irvine, CA; 3University of California Irvine Digestive Health Institute, Orange, CA; 4University of California Irvine Health, Orange, CA; 5University of California Irvine Digestive Health Institute, Exeter, CA
Introduction: Cirrhosis may lead to portal hypertension, which increases the risk of complications such as variceal bleeding. Pregnancy is a condition that is also associated with portal hypertension, as physiological hemodynamic changes worsen portal pressures and increase the risk of variceal bleed. In cirrhotic patients who are pregnant, it is imperative to monitor these patients closely and use a careful interdisciplinary approach. Here we describe the case of a pregnant female with variceal bleeding.
Case Description/Methods: A 35-year-old pregnant female with cirrhosis secondary to congenital biliary atresia with Kasai procedure presented at 26 weeks and 5 days gestation for bloody emesis. She had a prior pregnancy 13 years ago with fetal demise at 30 weeks in the setting variceal bleed. She had an EGD three months prior which demonstrated no varices. She was hemodynamically stable on admission. Fetal heart monitoring was normal. She was started on a PPI, octreotide, and ceftriaxone. Urgent EGD was done which demonstrated three medium sized varices, two with white nipple sign, that were banded as well as gastric varices with red-wale sign. Subsequently, a multidisciplinary meeting was held with Gastroenterology/Hepatology, Interventional Radiology, and Obstetrics. The Obstetrics team planned for tentative delivery at 28 weeks gestation given significant mortality risk of esophageal varices as well as a possible TIPS at 30 weeks gestation. A repeat EGD with EUS was done a week into her admission to reassess and measure portal pressure gradients. No varices were seen on the repeat endoscopy. Given these findings, the plan shifted to weekly EGD surveillance with portal vein pressure measurements to aid in decision making regarding the timing of the patient’s delivery. The following repeat endoscopies demonstrated no varices. She delivered at 32 weeks via cesarean section with no complications and was started on carvedilol for variceal prophylaxis.
Discussion: The goal of variceal surveillance in this patient was to evaluate the possible need for delivery prior to 32 weeks gestation. This case highlights the importance of vigilant and collaborative interdisciplinary care in pregnant cirrhotic patients, as well as a unique approach to determining the need for early delivery via cesarean section via serial endoscopies with concomitant portal pressure gradient measurements. Current guidelines suggest that variceal screening should be done in the second trimester in patients with suspected portal hypertension.
Disclosures:
Momin Masroor indicated no relevant financial relationships.
Sophie Trujillo indicated no relevant financial relationships.
Erica Duh indicated no relevant financial relationships.
Christina Ling indicated no relevant financial relationships.
Simon Long indicated no relevant financial relationships.
Usman Rahim indicated no relevant financial relationships.
Jason Samarasena: Cook Medical – Consultant. Medtronic – Advisory Committee/Board Member, Consultant. Neptune Medical – Advisory Committee/Board Member, Consultant. Olympus – Advisory Committee/Board Member, Consultant. Ovesco – Advisory Committee/Board Member, Consultant, Speakers Bureau. SatisfAI – Stock-privately held company. Steris – Advisory Committee/Board Member.
Momin Masroor, MD1, Sophie Trujillo, DO2, Erica Duh, MD3, Christina Ling, MD1, Simon Long, MD4, Usman Rahim, MD5, Jason Samarasena, MD1. P3066 - Pregnancy Under Pressure: Addressing Variceal Bleeding During Gestation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
