Monday Poster Session
Category: Liver
P3069 - The Shroom of Doom: Acute Liver Injury from Death Cap Mushroom Ingestion Treated With Experimental IV Silibinin
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Swapnil Patel, DO
Penn State Health Milton S. Hershey Medical Center
Hummelstown, PA
Presenting Author(s)
Swapnil Patel, DO1, Karen Krok, MD, FACG2
1Penn State Health Milton S. Hershey Medical Center, Hummelstown, PA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Amanita Phalloides (“Death Cap”) mushroom ingestion has been identified as one of the most common and deadly types of mushroom poisoning in the world due to the hepatotoxic effects of Amanita toxin. Many of these cases have rapidly progressed from acute liver injury to fulminant liver failure requiring orthotopic liver transplant. This case report describes the successful treatment of acute liver injury with prompt initiation of experimental IV silibinin after consumption of wild Amanita Phalloides mushrooms.
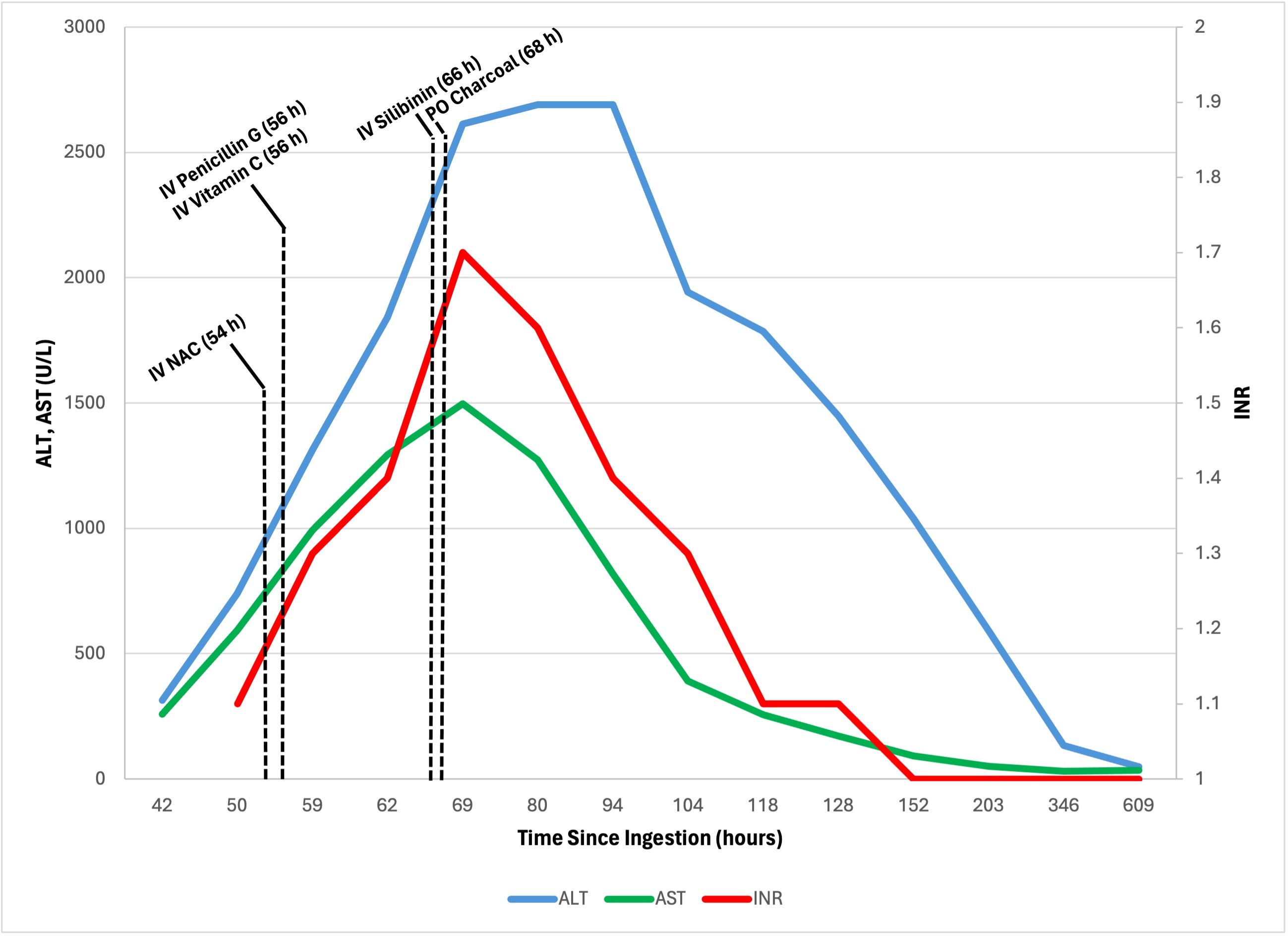
Case Description/Methods: A 60-year-old male with a history of hypothyroidism presented to an outpatient clinic with one day of vomiting, diarrhea, and epigastric pain. Approximately 48 hours earlier, he reported eating two wild mushrooms found in the woods in a homemade soup. Initial lab values were remarkable for creatinine 3.74 mg/dL (elevated from baseline), ALT 313 U/L, and AST 259 U/L. He was sent to the ED where poison control confirmed Amanita Phalloides poisoning based on the mushroom description by the patient. Treatment was initiated with IV fluids, IV N-acetylcysteine, IV vitamin C, activated oral charcoal, IV penicillin G, and IV silibinin (obtained via emergent FDA authorization). Lab testing for various infections and autoimmune markers were negative. Peak lab values during hospitalization are shown in Figure 1. He was continued on IV silibinin for a total of 3 days with clinical improvement and discharged 7 days after initial ingestion. Evaluation post-discharge showed improvement in ALT, AST, and INR as shown in Figure 1.
Discussion: In many instances Amanita Phalloides mushroom identification is not available acutely, but treatment should still be initiated promptly upon consultation with poison control. Treatment usually consists of supportive care, toxin elimination with activated charcoal, antioxidant therapy with N-acetylcysteine and vitamin C, and Amatoxin hepatocyte uptake inhibition with penicillin G and silibinin. Intravenous infusion of silibinin, an extract of milk thistle, is an experimental but preferred therapy that has been shown to improve mortality in patients with Amanita mushroom ingestion. Although silibinin is noted to be most effective when given within 24 hours after ingestion, this case shows clinical improvement when first administered >48 hours after ingestion of Amanita mushrooms. Timely recognition and treatment of Amanita mushroom poisoning is crucial to preventing acute liver failure and ultimately the need for an orthotopic liver transplant.
Disclosures:
Swapnil Patel, DO1, Karen Krok, MD, FACG2. P3069 - The Shroom of Doom: Acute Liver Injury from Death Cap Mushroom Ingestion Treated With Experimental IV Silibinin, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hummelstown, PA; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Amanita Phalloides (“Death Cap”) mushroom ingestion has been identified as one of the most common and deadly types of mushroom poisoning in the world due to the hepatotoxic effects of Amanita toxin. Many of these cases have rapidly progressed from acute liver injury to fulminant liver failure requiring orthotopic liver transplant. This case report describes the successful treatment of acute liver injury with prompt initiation of experimental IV silibinin after consumption of wild Amanita Phalloides mushrooms.
Case Description/Methods: A 60-year-old male with a history of hypothyroidism presented to an outpatient clinic with one day of vomiting, diarrhea, and epigastric pain. Approximately 48 hours earlier, he reported eating two wild mushrooms found in the woods in a homemade soup. Initial lab values were remarkable for creatinine 3.74 mg/dL (elevated from baseline), ALT 313 U/L, and AST 259 U/L. He was sent to the ED where poison control confirmed Amanita Phalloides poisoning based on the mushroom description by the patient. Treatment was initiated with IV fluids, IV N-acetylcysteine, IV vitamin C, activated oral charcoal, IV penicillin G, and IV silibinin (obtained via emergent FDA authorization). Lab testing for various infections and autoimmune markers were negative. Peak lab values during hospitalization are shown in Figure 1. He was continued on IV silibinin for a total of 3 days with clinical improvement and discharged 7 days after initial ingestion. Evaluation post-discharge showed improvement in ALT, AST, and INR as shown in Figure 1.
Discussion: In many instances Amanita Phalloides mushroom identification is not available acutely, but treatment should still be initiated promptly upon consultation with poison control. Treatment usually consists of supportive care, toxin elimination with activated charcoal, antioxidant therapy with N-acetylcysteine and vitamin C, and Amatoxin hepatocyte uptake inhibition with penicillin G and silibinin. Intravenous infusion of silibinin, an extract of milk thistle, is an experimental but preferred therapy that has been shown to improve mortality in patients with Amanita mushroom ingestion. Although silibinin is noted to be most effective when given within 24 hours after ingestion, this case shows clinical improvement when first administered >48 hours after ingestion of Amanita mushrooms. Timely recognition and treatment of Amanita mushroom poisoning is crucial to preventing acute liver failure and ultimately the need for an orthotopic liver transplant.
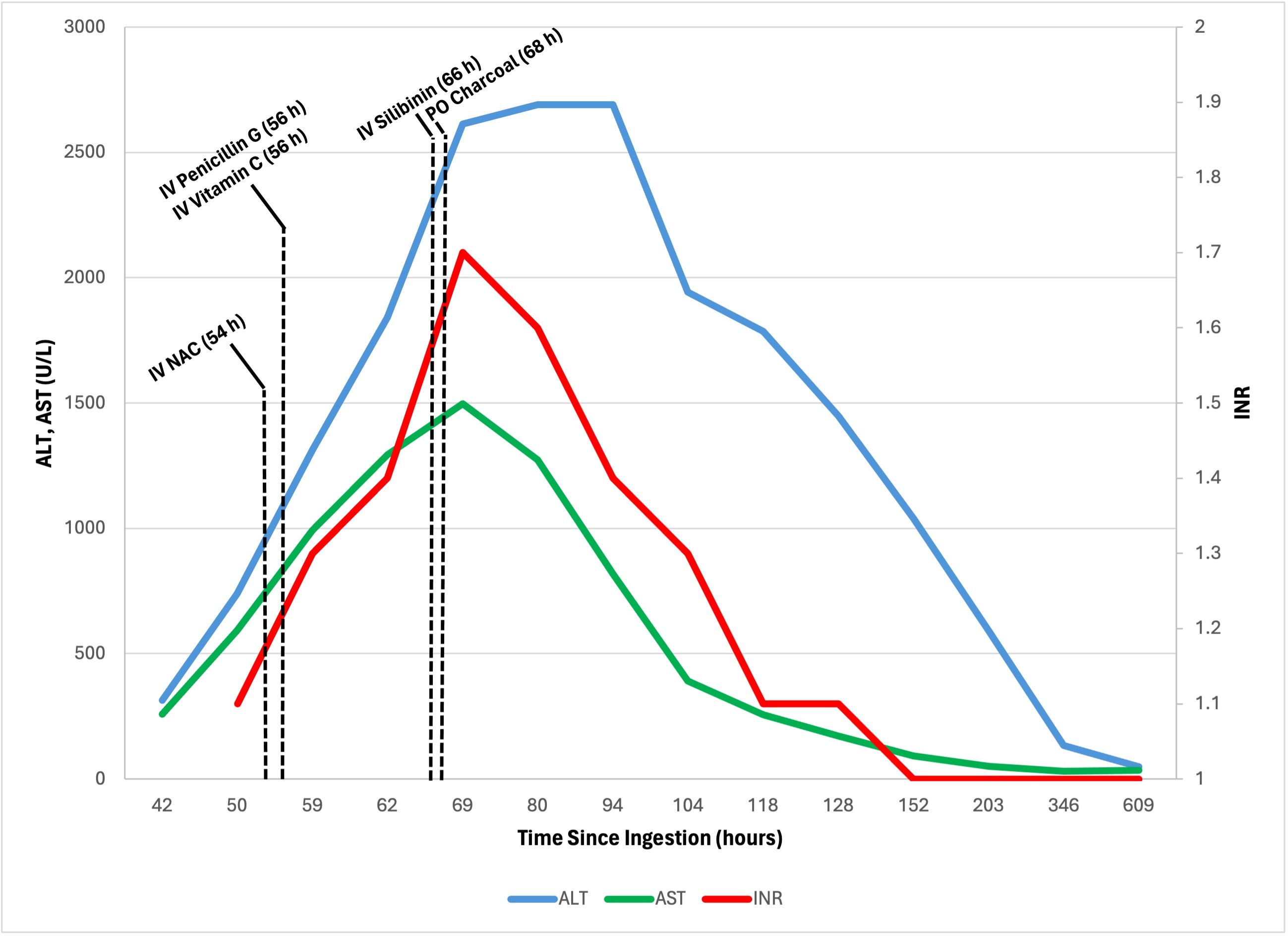
Figure: Figure 1. Trajectory of laboratory tests in relation to treatment interventions since the estimated time of mushroom ingestion. (ALT, alanine aminotransferase; AST, aspartate aminotransferase; INR, international normalized ratio; IV, intravenous; NAC, N-acetylcysteine; PO, per oral)
Disclosures:
Swapnil Patel indicated no relevant financial relationships.
Karen Krok indicated no relevant financial relationships.
Swapnil Patel, DO1, Karen Krok, MD, FACG2. P3069 - The Shroom of Doom: Acute Liver Injury from Death Cap Mushroom Ingestion Treated With Experimental IV Silibinin, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
