Monday Poster Session
Category: Liver
P3115 - Rare Case of Hemophagocytic Lmphohistiocytosis in a Post-Orthotopic Liver Transplant Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Parvir Aujla, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Parvir Aujla, MD1, Rohit Khanna, DO2, Abdullah S. Aleem, MD3, Alex Prevallet, DO4, Adam Deising, DO5
1University of Texas Health, McGovern Medical School, Houston, TX; 2Scripps Green Hospital, San Diego, CA; 3University of Texas at Houston, Houston, TX; 4HCA Riverside Community Hospital, Riverside, CA; 5Scripps Clinic Medical Group, La Jolla, CA
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare, life-threatening condition characterized by uncontrolled immune activation, hypercytokinemia, and hyperactivation of macrophages, often triggered by malignancy or infection. Here, we present a rare case of HLH in an adult male 20 days post-orthotopic liver transplant (OLT).
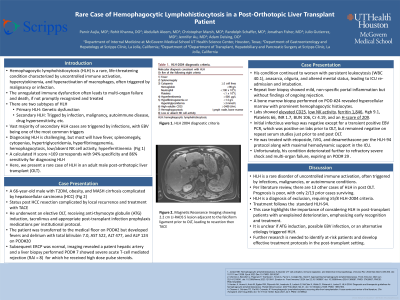
Case Description/Methods: A 66-year-old male with type 2 diabetes mellitus, obesity, and MASH cirrhosis complicated by hepatocellular carcinoma (HCC) with HCC resection complicated by local recurrence and treatment with TACE, underwent an elective OLT. He received two doses of antithymocyte globulin (ATG) post-transplant and was on tacrolimus, mycophenolate mofetil, fluconazole, TMP/SMX, and valganciclovir. Within two days, the patient was transferred to the medical floor but developed fevers and delirium with total bilirubin 7.0, AST 522, ALT 477, and ALP 124. Subsequent ERCP and liver biopsy was suggestive of severe acute T-cell mediated rejection for which he received high dose pulse steroids. His condition continued to worsen with persistent leukocytosis (WBC 40.1), anasarca, oliguria, and altered mental status, leading to ICU re-admission and intubation. Repeat liver biopsy showed mild, non-specific portal inflammation. A bone marrow biopsy, for suspicion of HLH, revealed hypercellular marrow with hemophagocytic histiocytes. Labs showed elevated CD25, low NK activity, ferritin 1,846, Hgb 9.1, Platelets 66, INR 1.7, BUN 106, Cr 4.19, and an H-score of 209. Infectious workup was negative except for a transient positive EBV PCR. He was treated with etoposide, IVIG, and dexamethasone per the HLH-94 protocol but developed DIC and septic shock, on four pressors with a lactate of 20, from VRE and Klebsiella oxytoca bacteremia. Unfortunately, he passed away 29 days post-OLT.
Discussion: HLH is a rare disorder of uncontrolled immune activation, often triggered by infections, malignancies, or autoimmune conditions. Per literature review, there are 13 other cases of HLH in post OLT. HLH is a diagnosis of exclusion, requiring ≥5/8 HLH-2004 criteria. Treatment follows the HLH-94. This case highlights the importance of considering HLH in post-transplant patients with unexplained deterioration, emphasizing early recognition and treatment. It is unclear if ATG induction, possible EBV infection, or an alternative etiology triggered HLH. Further research is needed to identify at-risk patients and develop effective treatment protocols in the post-transplant setting.
Disclosures:
Parvir Aujla, MD1, Rohit Khanna, DO2, Abdullah S. Aleem, MD3, Alex Prevallet, DO4, Adam Deising, DO5. P3115 - Rare Case of Hemophagocytic Lmphohistiocytosis in a Post-Orthotopic Liver Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2Scripps Green Hospital, San Diego, CA; 3University of Texas at Houston, Houston, TX; 4HCA Riverside Community Hospital, Riverside, CA; 5Scripps Clinic Medical Group, La Jolla, CA
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare, life-threatening condition characterized by uncontrolled immune activation, hypercytokinemia, and hyperactivation of macrophages, often triggered by malignancy or infection. Here, we present a rare case of HLH in an adult male 20 days post-orthotopic liver transplant (OLT).
Case Description/Methods: A 66-year-old male with type 2 diabetes mellitus, obesity, and MASH cirrhosis complicated by hepatocellular carcinoma (HCC) with HCC resection complicated by local recurrence and treatment with TACE, underwent an elective OLT. He received two doses of antithymocyte globulin (ATG) post-transplant and was on tacrolimus, mycophenolate mofetil, fluconazole, TMP/SMX, and valganciclovir. Within two days, the patient was transferred to the medical floor but developed fevers and delirium with total bilirubin 7.0, AST 522, ALT 477, and ALP 124. Subsequent ERCP and liver biopsy was suggestive of severe acute T-cell mediated rejection for which he received high dose pulse steroids. His condition continued to worsen with persistent leukocytosis (WBC 40.1), anasarca, oliguria, and altered mental status, leading to ICU re-admission and intubation. Repeat liver biopsy showed mild, non-specific portal inflammation. A bone marrow biopsy, for suspicion of HLH, revealed hypercellular marrow with hemophagocytic histiocytes. Labs showed elevated CD25, low NK activity, ferritin 1,846, Hgb 9.1, Platelets 66, INR 1.7, BUN 106, Cr 4.19, and an H-score of 209. Infectious workup was negative except for a transient positive EBV PCR. He was treated with etoposide, IVIG, and dexamethasone per the HLH-94 protocol but developed DIC and septic shock, on four pressors with a lactate of 20, from VRE and Klebsiella oxytoca bacteremia. Unfortunately, he passed away 29 days post-OLT.
Discussion: HLH is a rare disorder of uncontrolled immune activation, often triggered by infections, malignancies, or autoimmune conditions. Per literature review, there are 13 other cases of HLH in post OLT. HLH is a diagnosis of exclusion, requiring ≥5/8 HLH-2004 criteria. Treatment follows the HLH-94. This case highlights the importance of considering HLH in post-transplant patients with unexplained deterioration, emphasizing early recognition and treatment. It is unclear if ATG induction, possible EBV infection, or an alternative etiology triggered HLH. Further research is needed to identify at-risk patients and develop effective treatment protocols in the post-transplant setting.
Disclosures:
Parvir Aujla indicated no relevant financial relationships.
Rohit Khanna indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Alex Prevallet indicated no relevant financial relationships.
Adam Deising indicated no relevant financial relationships.
Parvir Aujla, MD1, Rohit Khanna, DO2, Abdullah S. Aleem, MD3, Alex Prevallet, DO4, Adam Deising, DO5. P3115 - Rare Case of Hemophagocytic Lmphohistiocytosis in a Post-Orthotopic Liver Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
