Monday Poster Session
Category: Liver
P3122 - Bile Duct Ballet: Dancing With Von Meyenburg Complexes and Liver Enzyme Riddles - Diagnostic Dilemma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Caleb Rashidian, DO
Prisma Health Greenville Memorial Hospital
Greenville, SC
Presenting Author(s)
Award: Presidential Poster Award
Caleb Rashidian, DO1, Anjani Jammula, MD2, Varun Moktan, MD3, Adrian Pona, DO1
1Prisma Health Greenville Memorial Hospital, Greenville, SC; 2Prisma Health, Greenville, SC; 3Prisma Health, University of South Carolina School of Medicine, Greenville, SC
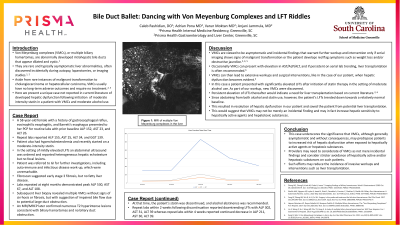
Introduction: Von Meyenburg complexes (VMCs), or multiple biliary hamartomas, are rare lesions often discovered incidentally during laparotomy or cross-sectional imaging, and often present with asymptomatic liver enzyme abnormalities. Characterized by dilated, cystic biliary ducts, VMCs can mimic metastatic liver disease and other liver pathologies, leading to extensive diagnostic evaluations and interventions.
Case Description/Methods: A 58-year-old female with a history of gastroesophageal reflux disease, eosinophilic esophagitis, and Barrett's esophagus, presented with newly diagnosed abnormal liver enzymes including aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline Phosphatase (ALP), and Gamma Glutamyl Transpeptidase (GGT). She denied a history of alcohol, herbal supplement use, viral, autoimmune hepatitis or familial liver disease. Abdominal ultrasound reported diffuse heterogeneous hepatic echotexture but no focal lesions. Further workup excluded autoimmune, and infectious etiologies, except for mildly elevated Alpha-1-Antitrypsin and actin antibodies. A Fibroscan was suggestive of stage 3 fibrosis but no fatty liver disease. Despite rising ALP, AST and ALT remained stable. Subsequent liver biopsy revealed VMCs without signs of autoimmune hepatitis or fibrosis, suggesting impaired bile flow due to large duct obstruction as the etiology of abnormal liver enzymes. An MRI later confirmed numerous T2 hyperintense lesions consistent with biliary hamartomas and no extrahepatic biliary duct obstruction.
Discussion: Although VMCs are typically incidental findings on imaging, liver biopsy remains the gold standard to confirm the diagnosis and rule out malignancy. VMCs can present with persistently elevated AST/ALT/ALP and are typically managed conservatively with serial observation/lab trending for their risk of transition to cholangiocarcinoma. The decision to pursue biopsy and possible resection is made when red flags such as weight loss or elevated tumor markers, are present. In cases with persistently elevated AST/ALT/ALP, liver transplantation is often considered; however, evidence for this recommendation is limited. This case underscores the significance of considering benign etiologies like VMCs in patients with unexplained liver enzyme elevation, particularly when initial workup is inconclusive.
Disclosures:
Caleb Rashidian, DO1, Anjani Jammula, MD2, Varun Moktan, MD3, Adrian Pona, DO1. P3122 - Bile Duct Ballet: Dancing With Von Meyenburg Complexes and Liver Enzyme Riddles - Diagnostic Dilemma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Caleb Rashidian, DO1, Anjani Jammula, MD2, Varun Moktan, MD3, Adrian Pona, DO1
1Prisma Health Greenville Memorial Hospital, Greenville, SC; 2Prisma Health, Greenville, SC; 3Prisma Health, University of South Carolina School of Medicine, Greenville, SC
Introduction: Von Meyenburg complexes (VMCs), or multiple biliary hamartomas, are rare lesions often discovered incidentally during laparotomy or cross-sectional imaging, and often present with asymptomatic liver enzyme abnormalities. Characterized by dilated, cystic biliary ducts, VMCs can mimic metastatic liver disease and other liver pathologies, leading to extensive diagnostic evaluations and interventions.
Case Description/Methods: A 58-year-old female with a history of gastroesophageal reflux disease, eosinophilic esophagitis, and Barrett's esophagus, presented with newly diagnosed abnormal liver enzymes including aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline Phosphatase (ALP), and Gamma Glutamyl Transpeptidase (GGT). She denied a history of alcohol, herbal supplement use, viral, autoimmune hepatitis or familial liver disease. Abdominal ultrasound reported diffuse heterogeneous hepatic echotexture but no focal lesions. Further workup excluded autoimmune, and infectious etiologies, except for mildly elevated Alpha-1-Antitrypsin and actin antibodies. A Fibroscan was suggestive of stage 3 fibrosis but no fatty liver disease. Despite rising ALP, AST and ALT remained stable. Subsequent liver biopsy revealed VMCs without signs of autoimmune hepatitis or fibrosis, suggesting impaired bile flow due to large duct obstruction as the etiology of abnormal liver enzymes. An MRI later confirmed numerous T2 hyperintense lesions consistent with biliary hamartomas and no extrahepatic biliary duct obstruction.
Discussion: Although VMCs are typically incidental findings on imaging, liver biopsy remains the gold standard to confirm the diagnosis and rule out malignancy. VMCs can present with persistently elevated AST/ALT/ALP and are typically managed conservatively with serial observation/lab trending for their risk of transition to cholangiocarcinoma. The decision to pursue biopsy and possible resection is made when red flags such as weight loss or elevated tumor markers, are present. In cases with persistently elevated AST/ALT/ALP, liver transplantation is often considered; however, evidence for this recommendation is limited. This case underscores the significance of considering benign etiologies like VMCs in patients with unexplained liver enzyme elevation, particularly when initial workup is inconclusive.
Disclosures:
Caleb Rashidian indicated no relevant financial relationships.
Anjani Jammula indicated no relevant financial relationships.
Varun Moktan indicated no relevant financial relationships.
Adrian Pona indicated no relevant financial relationships.
Caleb Rashidian, DO1, Anjani Jammula, MD2, Varun Moktan, MD3, Adrian Pona, DO1. P3122 - Bile Duct Ballet: Dancing With Von Meyenburg Complexes and Liver Enzyme Riddles - Diagnostic Dilemma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

