Monday Poster Session
Category: Liver
P3128 - Hemophagocytic Lymphohistiocytosis in Pregnancy Causing Clinically Significant Liver Dysfunction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Varun Vemulapalli, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Varun Vemulapalli, MD1, Cristina M. Natha, MD1, Prateek Harne, MD2, Asmeen Bhatt, MD3, Jenine Zaibaq-Krill, MD2
1University of Texas Health, McGovern Medical School, Houston, TX; 2The University of Texas Health Science Center, Houston, TX; 3Center for Interventional Gastroenterology at UTHealth (iGUT), Houston, TX
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare, immune-mediated condition of excessive inflammatory response with potential for multiorgan dysfunction (mortality of 41-75%). HLH in pregnancy in the setting of liver dysfunction can be difficult to diagnose due to its nonspecific presentation. The potential for severe complications highlights the need for timely diagnosis and treatment.
Case Description/Methods: A 38-year-old female with history of HSV infection presented at 19 weeks gestation with abdominal pain, vomiting, and jaundice. Labs revealed AST 5,780 U/L, alkaline phosphatase 142 U/L, total bilirubin 12 mg/dL, and INR 1.57. On hospital day four, total bilirubin and INR peaked at 28.6 mg/dL and 1.70, respectively. She did not have altered mental status throughout admission. Toxicity screen, infectious workup, and imaging were unremarkable. Further labs revealed ferritin >40,000 ng/mL and triglyceride 406 mg/dL. Oncology was consulted due to concern for HLH and started her on empiric therapy for HLH with dexamethasone. Subsequent liver biopsy confirmed HLH-induced acute hepatitis. The patient recovered well and was discharged on a steroid taper.
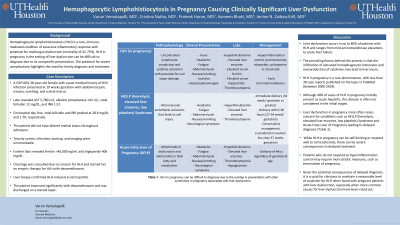
Discussion: Liver dysfunction occurs in up to 80% of patients with HLH and ranges from mild aminotransferase elevations to acute liver failure. The prevailing theory behind this process is that the infiltration of activated hemophagocytic histiocytes and overproduction of cytokines may lead to liver injury. HLH in pregnancy is a rare phenomenon, with less than 30 case reports published on the topic in PubMed (between 2000-2024). Although 40% of cases of HLH in pregnancy initially present as acute hepatitis, this disease is often not considered. Liver dysfunction in pregnancy more often raises concern for conditions such as HELLP (hemolysis, elevated liver enzymes, low platelets) Syndrome and Acute Fatty Liver of Pregnancy, leading to delayed diagnosis (Table 1). While HLH in pregnancy can be self-limiting or respond well to corticosteroids, there can be severe consequences to delayed treatment. Many case reports describe patients who do not respond to hyperinflammation control and require termination of pregnancy. One such patient was treated with corticosteroids and etoposide, required termination of pregnancy, and died despite these interventions. Given the potential consequences of delayed diagnosis, it is crucial for clinicians to maintain a reasonable level of suspicion for HLH when faced with pregnant patients with liver dysfunction.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Varun Vemulapalli, MD1, Cristina M. Natha, MD1, Prateek Harne, MD2, Asmeen Bhatt, MD3, Jenine Zaibaq-Krill, MD2. P3128 - Hemophagocytic Lymphohistiocytosis in Pregnancy Causing Clinically Significant Liver Dysfunction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2The University of Texas Health Science Center, Houston, TX; 3Center for Interventional Gastroenterology at UTHealth (iGUT), Houston, TX
Introduction: Hemophagocytic lymphohistiocytosis (HLH) is a rare, immune-mediated condition of excessive inflammatory response with potential for multiorgan dysfunction (mortality of 41-75%). HLH in pregnancy in the setting of liver dysfunction can be difficult to diagnose due to its nonspecific presentation. The potential for severe complications highlights the need for timely diagnosis and treatment.
Case Description/Methods: A 38-year-old female with history of HSV infection presented at 19 weeks gestation with abdominal pain, vomiting, and jaundice. Labs revealed AST 5,780 U/L, alkaline phosphatase 142 U/L, total bilirubin 12 mg/dL, and INR 1.57. On hospital day four, total bilirubin and INR peaked at 28.6 mg/dL and 1.70, respectively. She did not have altered mental status throughout admission. Toxicity screen, infectious workup, and imaging were unremarkable. Further labs revealed ferritin >40,000 ng/mL and triglyceride 406 mg/dL. Oncology was consulted due to concern for HLH and started her on empiric therapy for HLH with dexamethasone. Subsequent liver biopsy confirmed HLH-induced acute hepatitis. The patient recovered well and was discharged on a steroid taper.
Discussion: Liver dysfunction occurs in up to 80% of patients with HLH and ranges from mild aminotransferase elevations to acute liver failure. The prevailing theory behind this process is that the infiltration of activated hemophagocytic histiocytes and overproduction of cytokines may lead to liver injury. HLH in pregnancy is a rare phenomenon, with less than 30 case reports published on the topic in PubMed (between 2000-2024). Although 40% of cases of HLH in pregnancy initially present as acute hepatitis, this disease is often not considered. Liver dysfunction in pregnancy more often raises concern for conditions such as HELLP (hemolysis, elevated liver enzymes, low platelets) Syndrome and Acute Fatty Liver of Pregnancy, leading to delayed diagnosis (Table 1). While HLH in pregnancy can be self-limiting or respond well to corticosteroids, there can be severe consequences to delayed treatment. Many case reports describe patients who do not respond to hyperinflammation control and require termination of pregnancy. One such patient was treated with corticosteroids and etoposide, required termination of pregnancy, and died despite these interventions. Given the potential consequences of delayed diagnosis, it is crucial for clinicians to maintain a reasonable level of suspicion for HLH when faced with pregnant patients with liver dysfunction.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Varun Vemulapalli indicated no relevant financial relationships.
Cristina Natha indicated no relevant financial relationships.
Prateek Harne indicated no relevant financial relationships.
Asmeen Bhatt indicated no relevant financial relationships.
Jenine Zaibaq-Krill indicated no relevant financial relationships.
Varun Vemulapalli, MD1, Cristina M. Natha, MD1, Prateek Harne, MD2, Asmeen Bhatt, MD3, Jenine Zaibaq-Krill, MD2. P3128 - Hemophagocytic Lymphohistiocytosis in Pregnancy Causing Clinically Significant Liver Dysfunction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
