Monday Poster Session
Category: Liver
P3144 - Not DRESSed for Success: A Case of DRESS Syndrome With Progressively Elevated Aminotransferases Even After Stopping Offending Agent
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Manasa Vallabhaneni, MD
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Manasa Vallabhaneni, MD, Elizabeth Li, MD, Joanne Lin, DO, Kimberly Forde, MD, PhD, Carolyn Hogan, MD
Temple University Hospital, Philadelphia, PA
Introduction: Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a condition that leads to eosinophilia and systemic symptoms about 2-8 weeks after initiating a drug. It often resolves after stopping the offending agent and initiating steroid treatment. However, our case demonstrates an atypical presentation of increasing aminotransferases despite drug cessation.
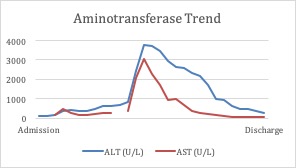
Case Description/Methods: A 31-year-old female with a history of intellectual disability, mood disorder, hypertension, and eczema presented to the hospital for a nonspecific diffuse whole-body rash. Her initial aminotransferase levels were elevated (ALT 97 U/L, AST 75 U/L) and CBC showed leukocytosis with eosinophilia. Acute viral hepatitis panel was negative. For her mood disorder, she was initiated on lamotrigine three weeks prior to admission. She was suspected to have DRESS syndrome secondary to lamotrigine. Dermatology recommended holding her lamotrigine and starting high-dose steroids. However, despite holding her lamotrigine for a week and initiation of steroids, her aminotransferases continued to rise (ALT 627 U/L, AST 267 U/L).
During the admission, the patient became febrile and tachycardic. Given the patient’s worsening clinical status and aminotransferase levels, an infectious work-up and liver biopsy were pursued. EBV, CMV, HSV, hepatitis B, and C viral loads were negative. She was started on N-acetylcysteine due to worsening liver synthetic function. Abdominal ultrasound Doppler was negative for thrombus. Biopsy showed preserved liver architecture with lobular inflammation and numerous eosinophils with negative HSV stains, pointing towards DRESS syndrome. Steroids were continued and lamotrigine was discontinued. Her laboratory results began to improve one month after discontinuation of lamotrigine and initiation of steroid treatment.
Discussion: This case highlights an unusual presentation of DRESS syndrome where the patient’s liver injury worsened after discontinuation of the offending agent and despite appropriate steroid treatment, persisted for weeks. It was further complicated by positive SIRS criteria, which pointed to a possible infectious etiology. There are few cases of severe liver injury due to DRESS syndrome; however, improvement is usually seen after a few days of steroid treatment. Our case shows that DRESS syndrome may not always result in an expected improvement in the aminotransferases after stopping the offending agent and further workup may be needed to confirm the diagnosis.
Disclosures:
Manasa Vallabhaneni, MD, Elizabeth Li, MD, Joanne Lin, DO, Kimberly Forde, MD, PhD, Carolyn Hogan, MD. P3144 - Not DRESSed for Success: A Case of DRESS Syndrome With Progressively Elevated Aminotransferases Even After Stopping Offending Agent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Temple University Hospital, Philadelphia, PA
Introduction: Drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome is a condition that leads to eosinophilia and systemic symptoms about 2-8 weeks after initiating a drug. It often resolves after stopping the offending agent and initiating steroid treatment. However, our case demonstrates an atypical presentation of increasing aminotransferases despite drug cessation.
Case Description/Methods: A 31-year-old female with a history of intellectual disability, mood disorder, hypertension, and eczema presented to the hospital for a nonspecific diffuse whole-body rash. Her initial aminotransferase levels were elevated (ALT 97 U/L, AST 75 U/L) and CBC showed leukocytosis with eosinophilia. Acute viral hepatitis panel was negative. For her mood disorder, she was initiated on lamotrigine three weeks prior to admission. She was suspected to have DRESS syndrome secondary to lamotrigine. Dermatology recommended holding her lamotrigine and starting high-dose steroids. However, despite holding her lamotrigine for a week and initiation of steroids, her aminotransferases continued to rise (ALT 627 U/L, AST 267 U/L).
During the admission, the patient became febrile and tachycardic. Given the patient’s worsening clinical status and aminotransferase levels, an infectious work-up and liver biopsy were pursued. EBV, CMV, HSV, hepatitis B, and C viral loads were negative. She was started on N-acetylcysteine due to worsening liver synthetic function. Abdominal ultrasound Doppler was negative for thrombus. Biopsy showed preserved liver architecture with lobular inflammation and numerous eosinophils with negative HSV stains, pointing towards DRESS syndrome. Steroids were continued and lamotrigine was discontinued. Her laboratory results began to improve one month after discontinuation of lamotrigine and initiation of steroid treatment.
Discussion: This case highlights an unusual presentation of DRESS syndrome where the patient’s liver injury worsened after discontinuation of the offending agent and despite appropriate steroid treatment, persisted for weeks. It was further complicated by positive SIRS criteria, which pointed to a possible infectious etiology. There are few cases of severe liver injury due to DRESS syndrome; however, improvement is usually seen after a few days of steroid treatment. Our case shows that DRESS syndrome may not always result in an expected improvement in the aminotransferases after stopping the offending agent and further workup may be needed to confirm the diagnosis.
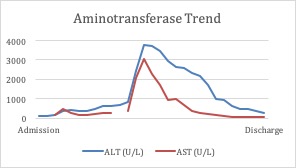
Figure: Graph 1: Trend of the patient’s aminotransferase levels from admission to discharge
Disclosures:
Manasa Vallabhaneni indicated no relevant financial relationships.
Elizabeth Li indicated no relevant financial relationships.
Joanne Lin indicated no relevant financial relationships.
Kimberly Forde indicated no relevant financial relationships.
Carolyn Hogan indicated no relevant financial relationships.
Manasa Vallabhaneni, MD, Elizabeth Li, MD, Joanne Lin, DO, Kimberly Forde, MD, PhD, Carolyn Hogan, MD. P3144 - Not DRESSed for Success: A Case of DRESS Syndrome With Progressively Elevated Aminotransferases Even After Stopping Offending Agent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
