Monday Poster Session
Category: Small Intestine
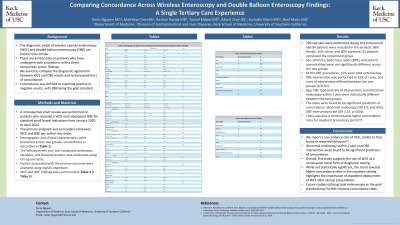
P3198 - Comparing Concordance Across Wireless Capsule Enteroscopy and Double Balloon Enteroscopy Findings: A Single Tertiary Care Referral Center Experience
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Denis Nguyen, MD
Keck School of Medicine of the University of Southern California
Los Angeles, CA
Presenting Author(s)
Denis Nguyen, MD1, Matthew Chen, BA2, Rachan Narala, MD1, Yousuf Kidwai, MD1, Albert Chen, BS3, Surinder Mann, MD1, Neel K. Mann, MD, MPH1
1Keck School of Medicine of the University of Southern California, Los Angeles, CA; 2Keck School of Medicine of the University of Southern California, Torrance, CA; 3California Institute of Technology, Los Angeles, CA
Introduction: The diagnostic yields of wireless capsule enteroscopy (WCE) and double balloon enteroscopy (DBE) are known to be similar. However, there is limited data on patients who have undergone both procedures with a direct comparison between findings. We aimed to compare the diagnostic agreement between WCE and DBE results and analyze predictors of concordance. Concordance was defined as matching positive or negative results, with DBE being the gold standard.
Methods: A retrospective chart review was performed on patients who received a WCE and subsequent DBE for standard small bowel indications from January 2020 to April 2024. The primary endpoint was concordance between WCE and DBE per author discretion.
Demographic and clinical characteristics were presented across two groups: concordance vs discordance (Table 1a). The Wilcoxon rank-sum test compared continuous variables, and bivariate analysis was conducted using Chi-square tests. Factors associated with the primary outcome were assessed using logistic regression (Table 1b), and WCE and DBE findings were summarized (Table 1c &1d).
Results: 790 capsules were performed during this time period and 84 patients were included in the analysis: 56% female, 36% white, and 60% inpatient. 63 patients composed the concordant group. Sex, ethnicity, and body mass index (BMI), and patient comorbidities were not significantly different across the two groups.
Of the DBE procedures, 15% were total enteroscopy. DBE intervention was performed in 55% of cases, and rates of intervention differed between the two groups (p< 0.02).
Age, DBE type and rate of intervention, and abnormal endoscopy within 1 year were statistically different between the two groups. The latter were found to be significant predictors of concordance: abnormal endoscopy (OR 5.0, p=0.005), DBE intervention rate (OR 3.25, p=0.04). There was also a trend towards higher concordance rates for inpatient procedures (p< 0.07).
Discussion: We report a concordance rate of 75%, similar to reported literature. Abnormal endoscopy within 1 year and DBE intervention were found to be significant predictors of concordance. Overall, this study supports the use of WCE as a noninvasive initial form of diagnostic testing. While not statistically significant, the trend towards higher concordance rates in the inpatient setting highlights the importance of expedient deployment of WCE after clinical presentation. Further studies utilizing total enteroscopy as the gold standard may raise concordance rates further.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Denis Nguyen, MD1, Matthew Chen, BA2, Rachan Narala, MD1, Yousuf Kidwai, MD1, Albert Chen, BS3, Surinder Mann, MD1, Neel K. Mann, MD, MPH1. P3198 - Comparing Concordance Across Wireless Capsule Enteroscopy and Double Balloon Enteroscopy Findings: A Single Tertiary Care Referral Center Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Keck School of Medicine of the University of Southern California, Los Angeles, CA; 2Keck School of Medicine of the University of Southern California, Torrance, CA; 3California Institute of Technology, Los Angeles, CA
Introduction: The diagnostic yields of wireless capsule enteroscopy (WCE) and double balloon enteroscopy (DBE) are known to be similar. However, there is limited data on patients who have undergone both procedures with a direct comparison between findings. We aimed to compare the diagnostic agreement between WCE and DBE results and analyze predictors of concordance. Concordance was defined as matching positive or negative results, with DBE being the gold standard.
Methods: A retrospective chart review was performed on patients who received a WCE and subsequent DBE for standard small bowel indications from January 2020 to April 2024. The primary endpoint was concordance between WCE and DBE per author discretion.
Demographic and clinical characteristics were presented across two groups: concordance vs discordance (Table 1a). The Wilcoxon rank-sum test compared continuous variables, and bivariate analysis was conducted using Chi-square tests. Factors associated with the primary outcome were assessed using logistic regression (Table 1b), and WCE and DBE findings were summarized (Table 1c &1d).
Results: 790 capsules were performed during this time period and 84 patients were included in the analysis: 56% female, 36% white, and 60% inpatient. 63 patients composed the concordant group. Sex, ethnicity, and body mass index (BMI), and patient comorbidities were not significantly different across the two groups.
Of the DBE procedures, 15% were total enteroscopy. DBE intervention was performed in 55% of cases, and rates of intervention differed between the two groups (p< 0.02).
Age, DBE type and rate of intervention, and abnormal endoscopy within 1 year were statistically different between the two groups. The latter were found to be significant predictors of concordance: abnormal endoscopy (OR 5.0, p=0.005), DBE intervention rate (OR 3.25, p=0.04). There was also a trend towards higher concordance rates for inpatient procedures (p< 0.07).
Discussion: We report a concordance rate of 75%, similar to reported literature. Abnormal endoscopy within 1 year and DBE intervention were found to be significant predictors of concordance. Overall, this study supports the use of WCE as a noninvasive initial form of diagnostic testing. While not statistically significant, the trend towards higher concordance rates in the inpatient setting highlights the importance of expedient deployment of WCE after clinical presentation. Further studies utilizing total enteroscopy as the gold standard may raise concordance rates further.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Denis Nguyen indicated no relevant financial relationships.
Matthew Chen indicated no relevant financial relationships.
Rachan Narala indicated no relevant financial relationships.
Yousuf Kidwai indicated no relevant financial relationships.
Albert Chen indicated no relevant financial relationships.
Surinder Mann indicated no relevant financial relationships.
Neel Mann indicated no relevant financial relationships.
Denis Nguyen, MD1, Matthew Chen, BA2, Rachan Narala, MD1, Yousuf Kidwai, MD1, Albert Chen, BS3, Surinder Mann, MD1, Neel K. Mann, MD, MPH1. P3198 - Comparing Concordance Across Wireless Capsule Enteroscopy and Double Balloon Enteroscopy Findings: A Single Tertiary Care Referral Center Experience, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
