Monday Poster Session
Category: Small Intestine
P3201 - Correlation of Non-Invasive Measurement With Gross Measurement of Small Bowel Length: A Meta-Analysis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nina Quirk, MS, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Nina Quirk, MS, MD1, Faisal Ali, MD2, Andrew Dupont, MD, MSPH3
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas, Houston, TX; 3McGovern Medical School at UTHealth, Houston, TX
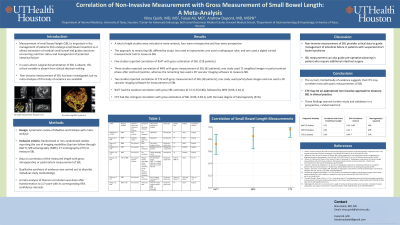
Introduction: Measurement of small bowel length (SBL) is important in the management of patients that undergo small bowel resection as it allows estimation of residual small bowel and guides decisions concerning nutrition status and management of potential intestinal failure. In cases where surgical documentation of SBL is absent, this critical variable is absent from clinical decision making. Non-invasive measurement of SBL has been investigated, but no meta-analyses of this body of evidence are available.
Methods: A systematic review of Medline and Embase was conducted to identify studies reporting the use of imaging modalities (barium follow-through; BaFT; MR enterography; MRE; CT enterography; CTE) to measure SBL and reporting correlation of the measured length with gross measurement of SBL (intra-operatively or post-mortem). Qualitative synthesis of evidence was carried out to describe individual study methodology. A meta-analysis of Pearson correlation was done after transformation to a Z score with its corresponding confidence intervals.
Results: A total of eight studies were included in this meta-analysis, none were randomized controlled trials. Five studies reported correlation of BaFT with gross estimation of SBL (118 patients). The approach to measuring SBL differed by study; two used an opisometer, one used a radiopaque ruler, and one used a digital curved measurement tool to measure SBL. Three studies reported correlation of MRE with gross measurement of SBL (82 patients); one study used T1-weighted images in portal contrast phase after contrast injection, whereas the remaining two used a 3D vascular imaging software to measure SBL. Two studies reported correlation of CTE with gross measurement of SBL (48 patients); one study used portal phase images and one used a 3D vascular imaging software for measurement of SBL.
BaFT had the weakest correlation with gross SBL estimates (0.72; 0.55,0.88), followed by MRE (0.85; 0.64,1). CTE had the strongest correlation with gross estimation of SBL (0.96; 0.83,1) with the least degree of heterogeneity (31%).
Discussion: The current, limited body of evidence suggests that CTE may correlate most with gross measurements of SBL. As such, CTE may be an appropriate non-invasive approach to measure SBL in clinical practice. These findings warrant further study and validation in a prospective, randomized trial.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nina Quirk, MS, MD1, Faisal Ali, MD2, Andrew Dupont, MD, MSPH3. P3201 - Correlation of Non-Invasive Measurement With Gross Measurement of Small Bowel Length: A Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas, Houston, TX; 3McGovern Medical School at UTHealth, Houston, TX
Introduction: Measurement of small bowel length (SBL) is important in the management of patients that undergo small bowel resection as it allows estimation of residual small bowel and guides decisions concerning nutrition status and management of potential intestinal failure. In cases where surgical documentation of SBL is absent, this critical variable is absent from clinical decision making. Non-invasive measurement of SBL has been investigated, but no meta-analyses of this body of evidence are available.
Methods: A systematic review of Medline and Embase was conducted to identify studies reporting the use of imaging modalities (barium follow-through; BaFT; MR enterography; MRE; CT enterography; CTE) to measure SBL and reporting correlation of the measured length with gross measurement of SBL (intra-operatively or post-mortem). Qualitative synthesis of evidence was carried out to describe individual study methodology. A meta-analysis of Pearson correlation was done after transformation to a Z score with its corresponding confidence intervals.
Results: A total of eight studies were included in this meta-analysis, none were randomized controlled trials. Five studies reported correlation of BaFT with gross estimation of SBL (118 patients). The approach to measuring SBL differed by study; two used an opisometer, one used a radiopaque ruler, and one used a digital curved measurement tool to measure SBL. Three studies reported correlation of MRE with gross measurement of SBL (82 patients); one study used T1-weighted images in portal contrast phase after contrast injection, whereas the remaining two used a 3D vascular imaging software to measure SBL. Two studies reported correlation of CTE with gross measurement of SBL (48 patients); one study used portal phase images and one used a 3D vascular imaging software for measurement of SBL.
BaFT had the weakest correlation with gross SBL estimates (0.72; 0.55,0.88), followed by MRE (0.85; 0.64,1). CTE had the strongest correlation with gross estimation of SBL (0.96; 0.83,1) with the least degree of heterogeneity (31%).
Discussion: The current, limited body of evidence suggests that CTE may correlate most with gross measurements of SBL. As such, CTE may be an appropriate non-invasive approach to measure SBL in clinical practice. These findings warrant further study and validation in a prospective, randomized trial.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nina Quirk indicated no relevant financial relationships.
Faisal Ali indicated no relevant financial relationships.
Andrew Dupont indicated no relevant financial relationships.
Nina Quirk, MS, MD1, Faisal Ali, MD2, Andrew Dupont, MD, MSPH3. P3201 - Correlation of Non-Invasive Measurement With Gross Measurement of Small Bowel Length: A Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
