Monday Poster Session
Category: Small Intestine
P3202 - Risk of Small Intestine Cancer in Inflammatory Bowel Disease: Results From A Large Multi-Center Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Saqr Alsakarneh, MD
University of Missouri - Kansas City School of Medicine
Kansas City, MO
Presenting Author(s)
Award: Presidential Poster Award
Saqr Alsakarneh, MD1, Mohamed Ahmed, MD, MSc1, Samiya Azim, BA1, Jana G. Hashash, MD, MSc2, Francis A. Farraye, MD, MSc2, Hassan Ghoz, MD1
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Mayo Clinic, Jacksonville, FL
Introduction: Inflammatory bowel disease (IBD) is associated with an increased risk of malignancy. Small bowel carcinoma (SBC) is a rare type of cancer, representing only 1-5% of all gastrointestinal tract malignancies. Although IBD has been established as a risk factor for colorectal cancer, there was mixed evidence regarding the risk of SBC in patients with IBD. We aimed to investigate the incidence of SBC in patients with IBD in the US.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify patients ≥18 years with IBD. Patients in the IBD cohort were matched with patients without a history of IBD (non-IBD group) by using 1:1 propensity score matching. The primary outcome was the incidence of SBC in patients with IBD. Secondary outcomes included comparing SBC risk in IBD with subgroup analyses for UC and CD. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs was used to compare time-to-event rates at daily time intervals.
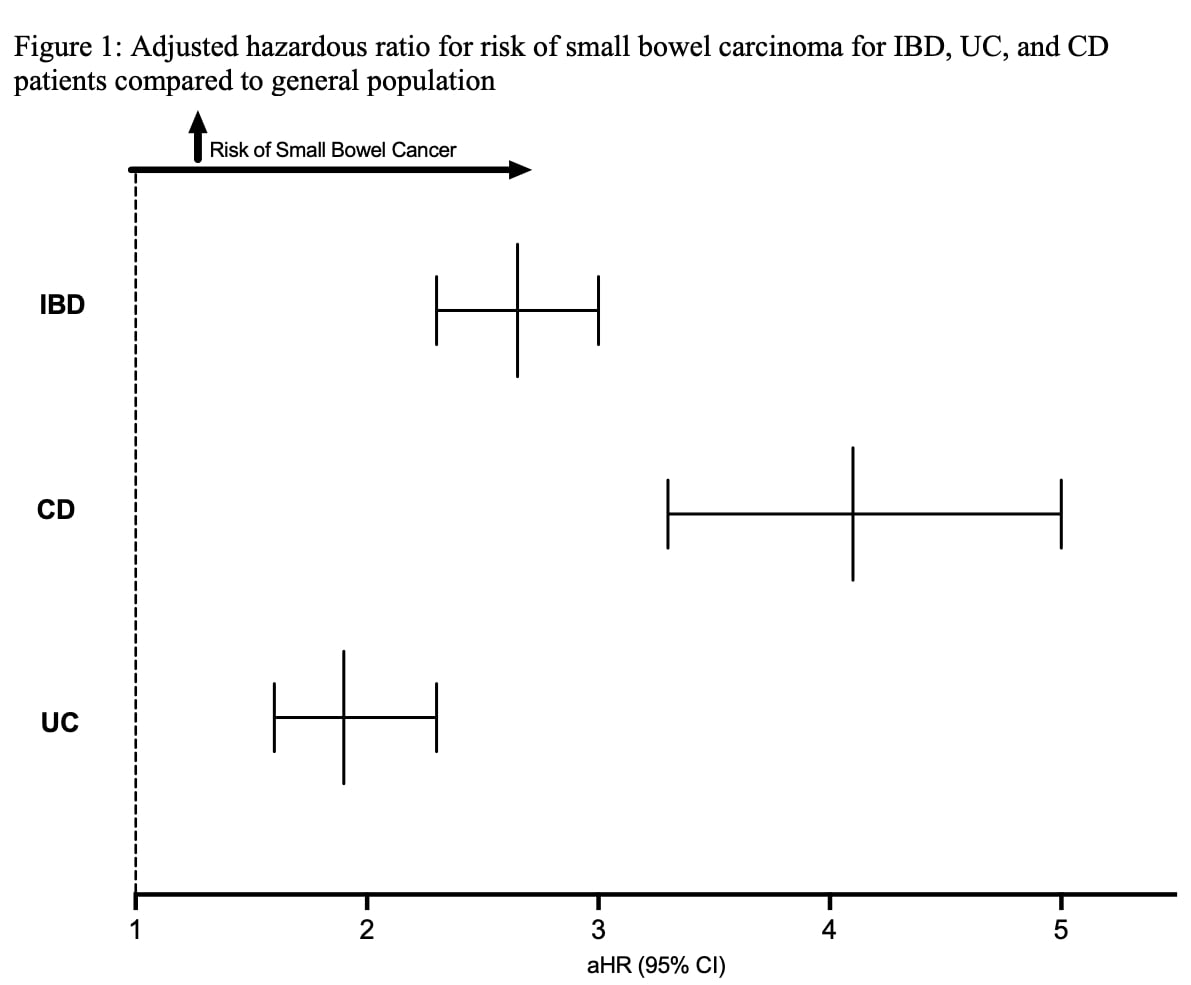
Results: Our cohort included 512,315 patients with IBD (mean age = 48 ± 19.4 years; 52.4% females). From 2010-2024, there was an increasing trend of SBC diagnosed in patients with IBD, with an Average Annual Percentage Change (AAPC) of 3.2% (P< 0.001). During the follow-up period, patients with IBD were at increased risk of SBC compared to the general population (aHR = 2.65; 95% CI: 2.31 - 3.04; P < .0001).
On a subgroup analysis, of 268,755 patients with CD, 586 were diagnosed with SBC during the follow-up, while among 280,051 patients with UC, only 343 patients were diagnosed with SBC. Patients with CD (aHR = 4.1; 95% CI: 3.38 – 4.99; P < .0001) had an increased risk of SBC compared to the general population without IBD, as well as patients with UC (aHR = 1.92; 95% CI: 1.6 – 2.33; P < .0001). All-cause mortality was higher in patients with both IBD and SBC compared to those with IBD without SBC (aHR = 2.7; 95% CI: 2.2 – 3.3; P < .0001).
Discussion: As far as we know, this is the first and largest real-world evidence from the US to show that IBD is an independent risk factor for SBC development. Patients with CD and, interestingly, UC had an elevated risk of developing SBC. Additionally, we found that there was an increasing trend of SBC in patients with IBD, which the improvement in endoscopic procedures and diagnostic modalities could partially explain. These results need validation from other data and study populations.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Saqr Alsakarneh, MD1, Mohamed Ahmed, MD, MSc1, Samiya Azim, BA1, Jana G. Hashash, MD, MSc2, Francis A. Farraye, MD, MSc2, Hassan Ghoz, MD1. P3202 - Risk of Small Intestine Cancer in Inflammatory Bowel Disease: Results From A Large Multi-Center Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Saqr Alsakarneh, MD1, Mohamed Ahmed, MD, MSc1, Samiya Azim, BA1, Jana G. Hashash, MD, MSc2, Francis A. Farraye, MD, MSc2, Hassan Ghoz, MD1
1University of Missouri - Kansas City School of Medicine, Kansas City, MO; 2Mayo Clinic, Jacksonville, FL
Introduction: Inflammatory bowel disease (IBD) is associated with an increased risk of malignancy. Small bowel carcinoma (SBC) is a rare type of cancer, representing only 1-5% of all gastrointestinal tract malignancies. Although IBD has been established as a risk factor for colorectal cancer, there was mixed evidence regarding the risk of SBC in patients with IBD. We aimed to investigate the incidence of SBC in patients with IBD in the US.
Methods: We conducted a retrospective cohort study using the TriNetX database to identify patients ≥18 years with IBD. Patients in the IBD cohort were matched with patients without a history of IBD (non-IBD group) by using 1:1 propensity score matching. The primary outcome was the incidence of SBC in patients with IBD. Secondary outcomes included comparing SBC risk in IBD with subgroup analyses for UC and CD. With censoring applied, Kaplan-Meier analysis with hazard ratios (HRs) and 95% CIs was used to compare time-to-event rates at daily time intervals.
Results: Our cohort included 512,315 patients with IBD (mean age = 48 ± 19.4 years; 52.4% females). From 2010-2024, there was an increasing trend of SBC diagnosed in patients with IBD, with an Average Annual Percentage Change (AAPC) of 3.2% (P< 0.001). During the follow-up period, patients with IBD were at increased risk of SBC compared to the general population (aHR = 2.65; 95% CI: 2.31 - 3.04; P < .0001).
On a subgroup analysis, of 268,755 patients with CD, 586 were diagnosed with SBC during the follow-up, while among 280,051 patients with UC, only 343 patients were diagnosed with SBC. Patients with CD (aHR = 4.1; 95% CI: 3.38 – 4.99; P < .0001) had an increased risk of SBC compared to the general population without IBD, as well as patients with UC (aHR = 1.92; 95% CI: 1.6 – 2.33; P < .0001). All-cause mortality was higher in patients with both IBD and SBC compared to those with IBD without SBC (aHR = 2.7; 95% CI: 2.2 – 3.3; P < .0001).
Discussion: As far as we know, this is the first and largest real-world evidence from the US to show that IBD is an independent risk factor for SBC development. Patients with CD and, interestingly, UC had an elevated risk of developing SBC. Additionally, we found that there was an increasing trend of SBC in patients with IBD, which the improvement in endoscopic procedures and diagnostic modalities could partially explain. These results need validation from other data and study populations.
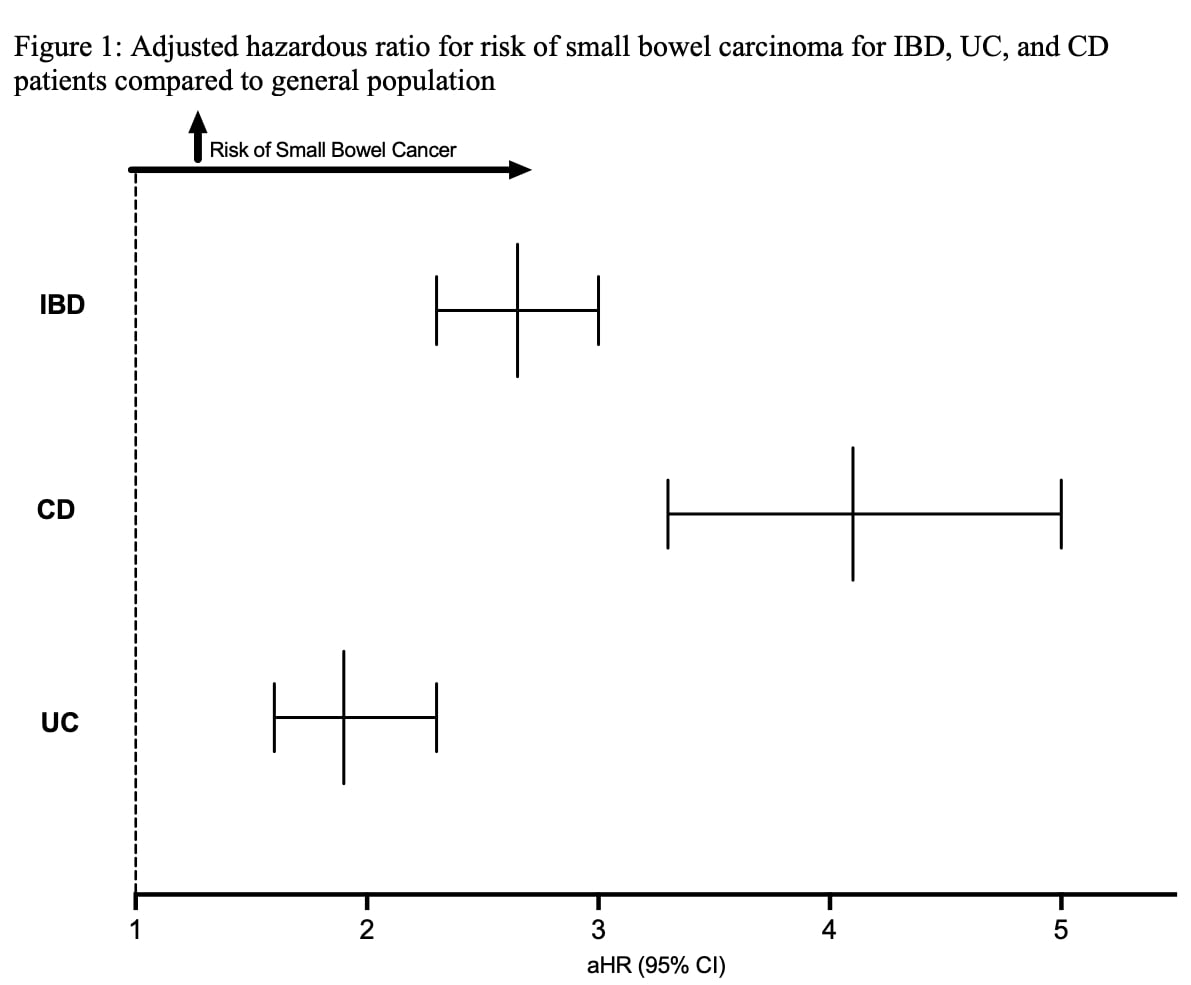
Figure: Figure 1: Adjusted hazardous ratio for risk of small bowel carcinoma for IBD, UC, and CD patients compared to the general population
Abbreviations: IBD: Inflammatory Bowel Disease; UC: Ulcerative Colitis; CD: Crohn's Disease
Abbreviations: IBD: Inflammatory Bowel Disease; UC: Ulcerative Colitis; CD: Crohn's Disease
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Mohamed Ahmed indicated no relevant financial relationships.
Samiya Azim indicated no relevant financial relationships.
Jana Hashash: Bristol Myers Squibb – Consultant.
Francis Farraye: AbbVie – Consultant. Avalo Therapeutics – Consultant. Bausch – Advisor or Review Panel Member. BMS – Consultant. Braintree Labs – Consultant. DSMB for Lilly. – Sits on. Fresenius Kabi – Consultant. GI Reviewers and IBD Educational Group – independent contractor. GSK, Iterative Health, Janssen, Pfizer, Pharmacosmos, Sandoz Immunology, Sebela and Viatris – Consultant.
Hassan Ghoz indicated no relevant financial relationships.
Saqr Alsakarneh, MD1, Mohamed Ahmed, MD, MSc1, Samiya Azim, BA1, Jana G. Hashash, MD, MSc2, Francis A. Farraye, MD, MSc2, Hassan Ghoz, MD1. P3202 - Risk of Small Intestine Cancer in Inflammatory Bowel Disease: Results From A Large Multi-Center Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

