Monday Poster Session
Category: Small Intestine
P3234 - A Case of Partial Duodenal Obstruction Secondary to Superior Mesenteric Artery Syndrome
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Jiteshwar S. Pannu, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Jiteshwar S. Pannu, MD1, Suparshva Parikh, MD1, Hemanth Sanjamala, MD1, Adolfo Diaz Barba, MD1, Zishan Mahmood, 2, Katy Adams, MD1, Salar Faiazi, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Superior Mesenteric Artery (SMA) Syndrome (also known as Wilkie’s Syndrome), is a rare clinical entity resulting from extrinsic compression of the 3rd part of duodenum due to a narrow aortomesenteric (AM) angle between the aorta and the SMA. Herein, we present a rare case of partial bowel obstruction due to SMA syndrome, managed conservatively with gastric decompression and nutritional optimization.
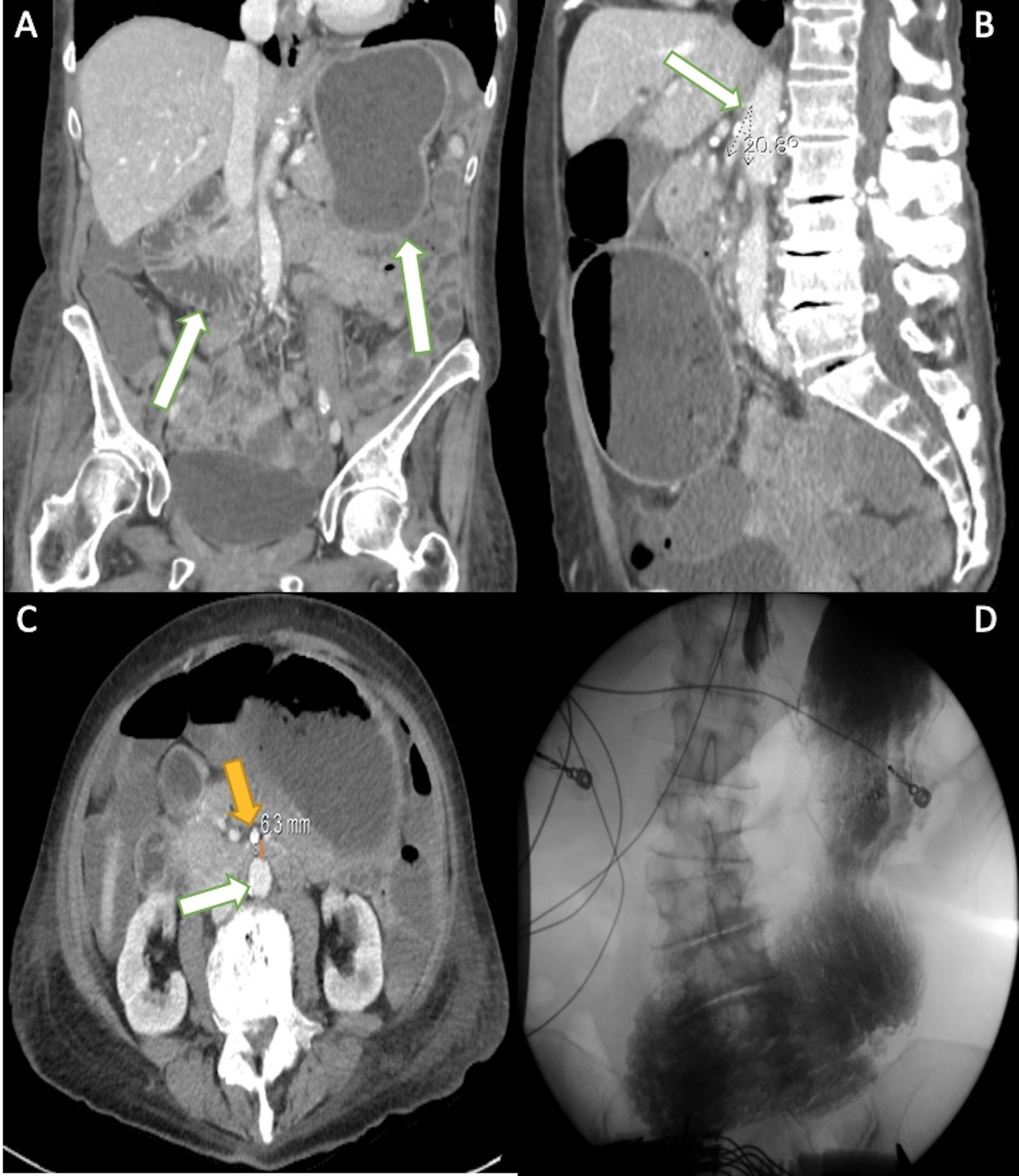
Case Description/Methods: A 69-year-old female with history of severe protein-calorie malnutrition, was admitted for generalized weakness, intermittent post-prandial nausea and epigastric abdominal pain. Physical exam revealed significant cachexia and a low BMI (17.1 kg/m2). Blood work was fairly unremarkable except Hb 8.9 and mild electrolyte derangements. CT abdomen with contrast revealed distended distal esophagus, stomach and proximal duodenum with extrinsic bowel compression within the narrow AM angle of 21 degree (N: 28-65 degree) and shortened AM distance of 6 mm (N: 10-34 mm), concerning for SMA syndrome. Findings were further correlated with an upper GI radiographic series. After multidisciplinary discussion involving minimally invasive surgery and gastroenterology, decision was made to pursue conservative management including nutritional optimization and gastric decompression. She responded well to this approach and was discharged with close follow up to assess the need for enteral feeding access and laparoscopic surgical repair in the future.
Discussion: With a low incidence of 0.1-0.3%, SMA syndrome can present numerous diagnostic challenges due to its vague clinical presentation. Pathophysiology involves narrowing of the AM angle secondary to reduction of mesenteric/retroperitoneal fat and rapid weight loss, leading to duodenal compression, which in turn leads to a vicious cycle of nutritional inadequacy and chronic abdominal symptoms. Other etiologies include anomalous insertion of Ligament of Treitz and post-surgical anatomical changes. Diagnosis rests on a high degree of clinical suspicion and cross sectional imaging (CT/MRI), and additional imaging such as barium swallow. Endoscopic evaluation may demonstrate pulsatile, extrinsic duodenal compression but its principal utility lies in establishing jejunal enteral access via naso-jejunal, PEG-J or PEJ tube. Surgical interventions such as entero-enterostomy and duodenal de-rotation are reserved for cases with failure of conservative management and complications such as complete bowel obstruction, perforation and ischemia.
Disclosures:
Jiteshwar S. Pannu, MD1, Suparshva Parikh, MD1, Hemanth Sanjamala, MD1, Adolfo Diaz Barba, MD1, Zishan Mahmood, 2, Katy Adams, MD1, Salar Faiazi, MD1. P3234 - A Case of Partial Duodenal Obstruction Secondary to Superior Mesenteric Artery Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2College of Medicine, University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Superior Mesenteric Artery (SMA) Syndrome (also known as Wilkie’s Syndrome), is a rare clinical entity resulting from extrinsic compression of the 3rd part of duodenum due to a narrow aortomesenteric (AM) angle between the aorta and the SMA. Herein, we present a rare case of partial bowel obstruction due to SMA syndrome, managed conservatively with gastric decompression and nutritional optimization.
Case Description/Methods: A 69-year-old female with history of severe protein-calorie malnutrition, was admitted for generalized weakness, intermittent post-prandial nausea and epigastric abdominal pain. Physical exam revealed significant cachexia and a low BMI (17.1 kg/m2). Blood work was fairly unremarkable except Hb 8.9 and mild electrolyte derangements. CT abdomen with contrast revealed distended distal esophagus, stomach and proximal duodenum with extrinsic bowel compression within the narrow AM angle of 21 degree (N: 28-65 degree) and shortened AM distance of 6 mm (N: 10-34 mm), concerning for SMA syndrome. Findings were further correlated with an upper GI radiographic series. After multidisciplinary discussion involving minimally invasive surgery and gastroenterology, decision was made to pursue conservative management including nutritional optimization and gastric decompression. She responded well to this approach and was discharged with close follow up to assess the need for enteral feeding access and laparoscopic surgical repair in the future.
Discussion: With a low incidence of 0.1-0.3%, SMA syndrome can present numerous diagnostic challenges due to its vague clinical presentation. Pathophysiology involves narrowing of the AM angle secondary to reduction of mesenteric/retroperitoneal fat and rapid weight loss, leading to duodenal compression, which in turn leads to a vicious cycle of nutritional inadequacy and chronic abdominal symptoms. Other etiologies include anomalous insertion of Ligament of Treitz and post-surgical anatomical changes. Diagnosis rests on a high degree of clinical suspicion and cross sectional imaging (CT/MRI), and additional imaging such as barium swallow. Endoscopic evaluation may demonstrate pulsatile, extrinsic duodenal compression but its principal utility lies in establishing jejunal enteral access via naso-jejunal, PEG-J or PEJ tube. Surgical interventions such as entero-enterostomy and duodenal de-rotation are reserved for cases with failure of conservative management and complications such as complete bowel obstruction, perforation and ischemia.
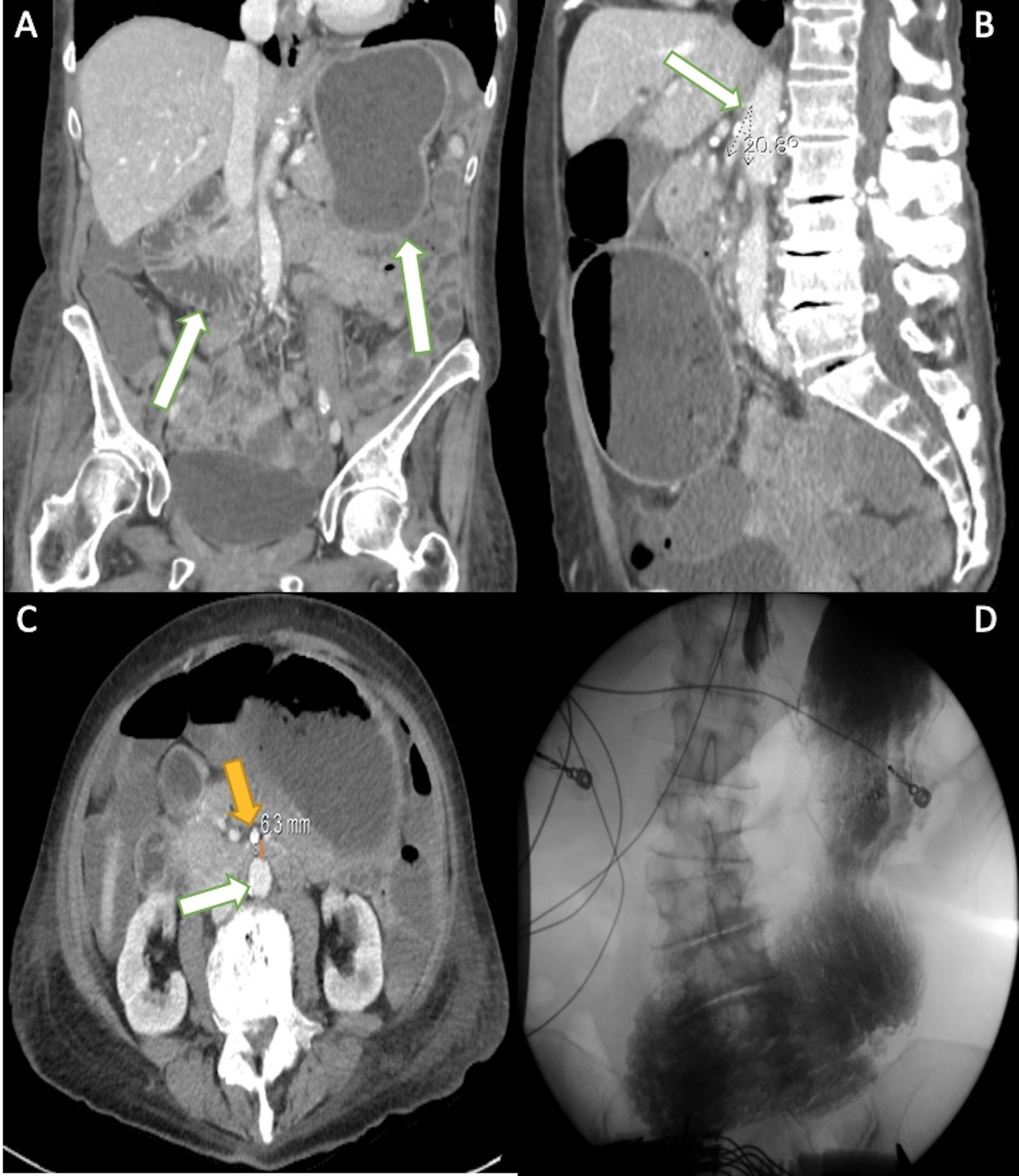
Figure: Figure A: CT abdomen with contrast revealing a distended stomach and proximal duodenum (white arrows);
Figure B: Narrow aorto-mesenteric (AM) angle of 21 degree (N: 28-65 degree) between the aorta and the SMA;
Figure C: Shortened aorto-mesenteric (AM) distance of 6 mm (N: 10-34 mm) between the aorta (white arrow) and the SMA (yellow arrow);
Figure D: Distended stomach and proximal duodenum seen on upper GI radiographic series;
Figure B: Narrow aorto-mesenteric (AM) angle of 21 degree (N: 28-65 degree) between the aorta and the SMA;
Figure C: Shortened aorto-mesenteric (AM) distance of 6 mm (N: 10-34 mm) between the aorta (white arrow) and the SMA (yellow arrow);
Figure D: Distended stomach and proximal duodenum seen on upper GI radiographic series;
Disclosures:
Jiteshwar Pannu indicated no relevant financial relationships.
Suparshva Parikh indicated no relevant financial relationships.
Hemanth Sanjamala indicated no relevant financial relationships.
Adolfo Diaz Barba indicated no relevant financial relationships.
Zishan Mahmood indicated no relevant financial relationships.
Katy Adams indicated no relevant financial relationships.
Salar Faiazi indicated no relevant financial relationships.
Jiteshwar S. Pannu, MD1, Suparshva Parikh, MD1, Hemanth Sanjamala, MD1, Adolfo Diaz Barba, MD1, Zishan Mahmood, 2, Katy Adams, MD1, Salar Faiazi, MD1. P3234 - A Case of Partial Duodenal Obstruction Secondary to Superior Mesenteric Artery Syndrome, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
