Monday Poster Session
Category: Small Intestine
P3239 - Necrotizing Abdominal Lymphadenopathy: A Rare Presentation of Whipple’s Disease Diagnosed on EUS-Guided Sampling of the Abdominal Lymph Nodes
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AM
Anila Mahesh, MD
Geisinger Wyoming Valley Medical Center
Wilkes-Barre, PA
Presenting Author(s)
Anila Mahesh, MD1, Deepak Kumar, MD2, Umar Hayat, MD1, Kishore Kumar, MD3
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Mather Hospital, Northwell Health, Port Jefferson, NY; 3Geisinger Community Medical Center, Scranton, PA
Introduction: Whipples disease (WD) is a rare, chronic multisystem disorder caused by a gram-positive bacillus, Tropheryma whipplei (TW). WD is seen in Caucasian with a male/female ratio of 4.1. Transmitted among humans via the feco-oral. Clinical manifestations are variable including diarrhea, weight loss, abdominal pain, fever, anorexia, steatorrhea, cachexia, arthralgia, lymphadenopathy and neurologic manifestation. The diagnosis is made by small bowel specimen histology with PAS staining, PCR testing, and immunohistochemistry. We describe a rare case of Whipple's disease in an intellectually disabled patient with symptoms of chronic diarrhea, weight loss, IDA and severe abdominal lymphadenopathy. The negative PCR of duodenal biopsy made diagnosis more challenging.
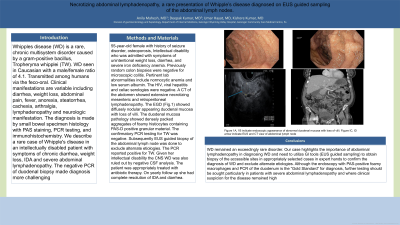
Case Description/Methods: 55-year-old female with history of seizure disorder, osteoporosis, Intellectual disability who was admitted with symptoms of unintentional weight loss, diarrhea, and severe iron deficiency anemia(IDA). Previously random colon biopsies were negative for microscopic colitis. Pertinent lab abnormalities include normocytic anemia and low serum albumin. The HIV, viral hepatitis and celiac serologies were negative. A CT of the abdomen showed extensive necrotizing mesenteric and retroperitoneal lymphadenopathy. The EGD showed diffusely nodular appearing duodenal mucosa with loss of villi. The duodenal mucosa pathology showed densely packed aggregates of foamy histiocytes containing PAS-D positive granular material. The confirmatory PCR testing for TW was negative. Subsequently EUS guided biopsy of the abdominal lymph node was done to exclude alternate etiologies. The PCR reported positive for TW. Given her intellectual disability the CNS WD was also ruled out by negative CSF analysis. The patient was appropriately treated with antibiotic therapy. On yearly follow up she had complete resolution of IDA and diarrhea.
Discussion: WD remained an exceedingly rare disorder. Our case highlights the importance of abdominal lymphadenopathy in diagnosing WD and need to utilize GI tools (EUS guided sampling) to obtain biopsy of the accessible sites in appropriately selected cases in expert hands to confirm the diagnosis of WD and exclude alternate etiologies. Although the endoscopy with PAS-positive foamy macrophages and PCR of the duodenum is the “Gold Standard” for diagnosis, further testing should be sought particularly in patients with severe abdominal lymphadenopathy and where clinical suspicion for the disease remained high.
Disclosures:
Anila Mahesh, MD1, Deepak Kumar, MD2, Umar Hayat, MD1, Kishore Kumar, MD3. P3239 - Necrotizing Abdominal Lymphadenopathy: A Rare Presentation of Whipple’s Disease Diagnosed on EUS-Guided Sampling of the Abdominal Lymph Nodes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Geisinger Wyoming Valley Medical Center, Wilkes-Barre, PA; 2Mather Hospital, Northwell Health, Port Jefferson, NY; 3Geisinger Community Medical Center, Scranton, PA
Introduction: Whipples disease (WD) is a rare, chronic multisystem disorder caused by a gram-positive bacillus, Tropheryma whipplei (TW). WD is seen in Caucasian with a male/female ratio of 4.1. Transmitted among humans via the feco-oral. Clinical manifestations are variable including diarrhea, weight loss, abdominal pain, fever, anorexia, steatorrhea, cachexia, arthralgia, lymphadenopathy and neurologic manifestation. The diagnosis is made by small bowel specimen histology with PAS staining, PCR testing, and immunohistochemistry. We describe a rare case of Whipple's disease in an intellectually disabled patient with symptoms of chronic diarrhea, weight loss, IDA and severe abdominal lymphadenopathy. The negative PCR of duodenal biopsy made diagnosis more challenging.
Case Description/Methods: 55-year-old female with history of seizure disorder, osteoporosis, Intellectual disability who was admitted with symptoms of unintentional weight loss, diarrhea, and severe iron deficiency anemia(IDA). Previously random colon biopsies were negative for microscopic colitis. Pertinent lab abnormalities include normocytic anemia and low serum albumin. The HIV, viral hepatitis and celiac serologies were negative. A CT of the abdomen showed extensive necrotizing mesenteric and retroperitoneal lymphadenopathy. The EGD showed diffusely nodular appearing duodenal mucosa with loss of villi. The duodenal mucosa pathology showed densely packed aggregates of foamy histiocytes containing PAS-D positive granular material. The confirmatory PCR testing for TW was negative. Subsequently EUS guided biopsy of the abdominal lymph node was done to exclude alternate etiologies. The PCR reported positive for TW. Given her intellectual disability the CNS WD was also ruled out by negative CSF analysis. The patient was appropriately treated with antibiotic therapy. On yearly follow up she had complete resolution of IDA and diarrhea.
Discussion: WD remained an exceedingly rare disorder. Our case highlights the importance of abdominal lymphadenopathy in diagnosing WD and need to utilize GI tools (EUS guided sampling) to obtain biopsy of the accessible sites in appropriately selected cases in expert hands to confirm the diagnosis of WD and exclude alternate etiologies. Although the endoscopy with PAS-positive foamy macrophages and PCR of the duodenum is the “Gold Standard” for diagnosis, further testing should be sought particularly in patients with severe abdominal lymphadenopathy and where clinical suspicion for the disease remained high.
Disclosures:
Anila Mahesh indicated no relevant financial relationships.
Deepak Kumar indicated no relevant financial relationships.
Umar Hayat indicated no relevant financial relationships.
Kishore Kumar indicated no relevant financial relationships.
Anila Mahesh, MD1, Deepak Kumar, MD2, Umar Hayat, MD1, Kishore Kumar, MD3. P3239 - Necrotizing Abdominal Lymphadenopathy: A Rare Presentation of Whipple’s Disease Diagnosed on EUS-Guided Sampling of the Abdominal Lymph Nodes, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
