Monday Poster Session
Category: Small Intestine
P3240 - Adult Megaduodenum Secondary to Short Bowel Syndrome Following Intestinal Resection for Congenital Jejunal Atresia
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ES
Eva Schaible, MD
Mayo Clinic School of Graduate Medical Education
Rochester, MN
Presenting Author(s)
Eva Schaible, MD1, Caroline Matchett, MD2, Karthik Ravi, MD2, Sara Bonnes, MD, MS2, Xiao Jing (Iris) Wang, MD2
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2Mayo Clinic, Rochester, MN
Introduction: Congenital intestinal atresia initially presents in infants with intestinal obstruction shortly after birth, requiring surgical resection of the affected bowel segments. Complications can arise depending on the amount of bowel that is resected. We present a case of short gut syndrome (SBS) in an adult man following significant bowel resection for jejunal atresia as an infant, complicated by multiple bowel obstructions progressing to megaduodenum.
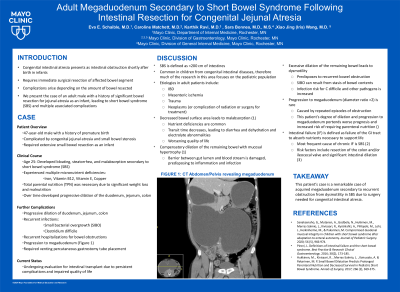
Case Description/Methods: Patient is a 47-year-old man with history of premature birth complicated by congenital jejunal atresia and stenosis of the small bowel (SB) requiring lengthy SB resection as an infant. The patient did well until age 25, when he presented with bloating, steatorrhea, and malnutrition with multiple micronutrient deficiencies (copper, Vitamin E, B12, iron) secondary to SBS. The patient then developed marked dilation of the duodenum, jejunum, and colon, complicated by recurrent episodes of small intestinal bacterial overgrowth (SIBO), Clostridium difficile infections, and worsening malabsorption. The patient continued to struggle with significant diarrhea, bloating, and vomiting, requiring Total Parenteral Nutrition (TPN) for intestinal failure. Despite times, patient had recurrent hospitalizations for bowel obstructions, progressive megaduodenum (Figure 1) from impaired intestinal motility, requiring venting percutaneous gastrostomy tube placement. Due to persistent complications and impaired quality of life, patient is undergoing evaluation for intestinal transplant.
Discussion: SBS (< 200 cm intestines), due to lack of adequate bowel surface area, leads to decreased absorption of nutrients and increased transit. The remaining intestines adapt, leading to compensatory dilation and mucosal hypertrophy. Excessive dilation can impair intestinal mobility and gut barrier function, further limiting intestinal function. Progression to megaduodenum (diameter ratio >2) is rare, and this patient’s case is remarkable with complications of recurrent obstruction from dysmotility. This degree of dilation portends a worse prognosis and predicts increased risk of requiring parenteral nutrition.

Disclosures:
Eva Schaible, MD1, Caroline Matchett, MD2, Karthik Ravi, MD2, Sara Bonnes, MD, MS2, Xiao Jing (Iris) Wang, MD2. P3240 - Adult Megaduodenum Secondary to Short Bowel Syndrome Following Intestinal Resection for Congenital Jejunal Atresia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2Mayo Clinic, Rochester, MN
Introduction: Congenital intestinal atresia initially presents in infants with intestinal obstruction shortly after birth, requiring surgical resection of the affected bowel segments. Complications can arise depending on the amount of bowel that is resected. We present a case of short gut syndrome (SBS) in an adult man following significant bowel resection for jejunal atresia as an infant, complicated by multiple bowel obstructions progressing to megaduodenum.
Case Description/Methods: Patient is a 47-year-old man with history of premature birth complicated by congenital jejunal atresia and stenosis of the small bowel (SB) requiring lengthy SB resection as an infant. The patient did well until age 25, when he presented with bloating, steatorrhea, and malnutrition with multiple micronutrient deficiencies (copper, Vitamin E, B12, iron) secondary to SBS. The patient then developed marked dilation of the duodenum, jejunum, and colon, complicated by recurrent episodes of small intestinal bacterial overgrowth (SIBO), Clostridium difficile infections, and worsening malabsorption. The patient continued to struggle with significant diarrhea, bloating, and vomiting, requiring Total Parenteral Nutrition (TPN) for intestinal failure. Despite times, patient had recurrent hospitalizations for bowel obstructions, progressive megaduodenum (Figure 1) from impaired intestinal motility, requiring venting percutaneous gastrostomy tube placement. Due to persistent complications and impaired quality of life, patient is undergoing evaluation for intestinal transplant.
Discussion: SBS (< 200 cm intestines), due to lack of adequate bowel surface area, leads to decreased absorption of nutrients and increased transit. The remaining intestines adapt, leading to compensatory dilation and mucosal hypertrophy. Excessive dilation can impair intestinal mobility and gut barrier function, further limiting intestinal function. Progression to megaduodenum (diameter ratio >2) is rare, and this patient’s case is remarkable with complications of recurrent obstruction from dysmotility. This degree of dilation portends a worse prognosis and predicts increased risk of requiring parenteral nutrition.

Figure: Figure 1. Computed tomography completed on admission for bowel obstruction, revealing significant megaduodenum leading to compression of other abdominal organs
Disclosures:
Eva Schaible indicated no relevant financial relationships.
Caroline Matchett indicated no relevant financial relationships.
Karthik Ravi indicated no relevant financial relationships.
Sara Bonnes: CorMedix – Advisor or Review Panel Member.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Eva Schaible, MD1, Caroline Matchett, MD2, Karthik Ravi, MD2, Sara Bonnes, MD, MS2, Xiao Jing (Iris) Wang, MD2. P3240 - Adult Megaduodenum Secondary to Short Bowel Syndrome Following Intestinal Resection for Congenital Jejunal Atresia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
