Monday Poster Session
Category: Small Intestine
P3245 - Gut Instincts: Navigating a Hidden Case of Gastrointestinal Amyloidosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Lawrence Zhou, MD
The University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Lawrence Zhou, MD1, Aastha V. Bharwad, MD2, Daly Al-Hadeethi, MD2, Rahul Shekhar, MD2, Andrew Osbeck, PA-C2, William Palko, MD3, Kyle Rowe, MD4, William J. Salyers, MD, MPH2
1The University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3Wesley Medical Center, Wichita, KS; 4University of Kansas Medical Center, Wichita, KS
Introduction: Amyloidosis encompasses disorders characterized by the misfolding and deposition of insoluble fibrils within organs causing dysfunction. GI involvement occurs in approximately 3% of cases, and overall less than 1% later also develop multiple myeloma (MM). Clinical manifestations are usually nonspecific such as chronic diarrhea, weight loss, abdominal pain, and bloating. We present a case of GI amyloidosis in the absence of MM.
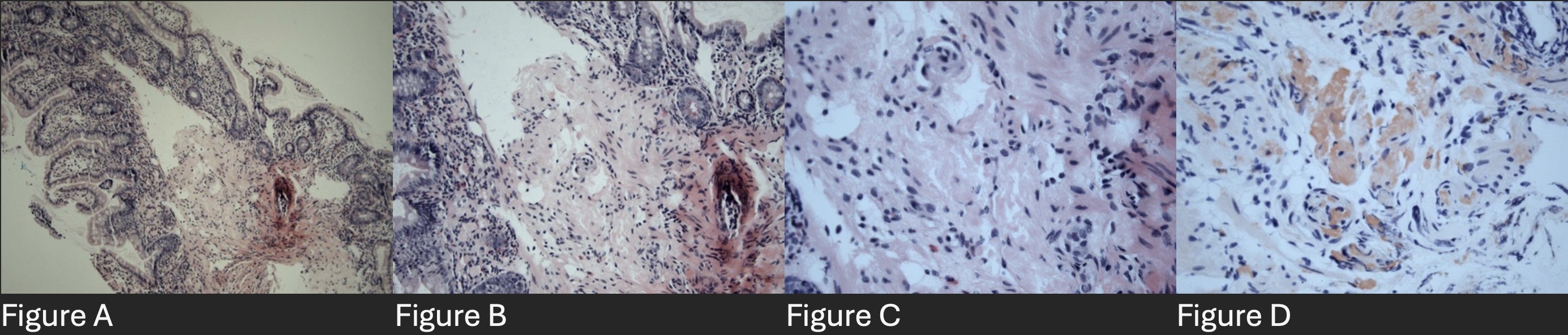
Case Description/Methods: A 61 year-old female with history of familial adenomatous polyposis status-post colectomy with ileostomy, and chronically high alkaline phosphatase (ALP) was admitted with diarrhea, dehydration and kidney injury. Labs were also significant for aspartate aminotransferase 75 U/L, alanine aminotransferase 117 U/L, ALP 1304 U/L, and gamma-glutamyl transpeptidase (GGT) 1174 U/L. Prior hepatitis workup was negative, and magnetic resonance cholangiopancreatography showed intra- and extrahepatic biliary dilatation and lack of smooth tapering, so outpatient liver biopsy was planned. Endoscopy was performed due to profuse diarrhea and biopsies showed a micro-globular pattern of amyloid deposition within the lamina propria and submucosa (Figure A-D).
Prior to following up on the findings of gastrointestinal amyloidosis, the patient was admitted for acute renal failure. Free light chains were elevated, but protein electrophoresis and serologies were negative. She was started on prednisone for suspected nephrotic syndrome and biopsy revealed light chain (AL) amyloidosis. ALP and GGT peaked at 4259 U/L and 1547 U/L respectively. She subsequently started hemodialysis.
Before she could see oncology, she was admitted for life-threatening hyperkalemia after missing dialysis. She was started on cyclophosphamide, bortezomib, and dexamethasone (CyBorD), but developed severe methicillin-resistant Staphylococcus aureus (MRSA) bacteremia and empyema leading to intubation. Unfortunately, she continued to decompensate and was ultimately placed on hospice.
Discussion: Intestinal involvement is rare, occurring typically as part of systemic amyloidosis. Hepatic amyloidosis should be suspected in patients with weight loss or hepatomegaly, along with elevated ALP, proteinuria, and signs of hyposplenism, but requires biopsy confirmation. This patient’s disease progressed to renal failure and was complicated by hyposplenism manifesting as MRSA infection. Although no therapies are approved for AL amyloidosis, CYBorD regimen is the standard treatment.
Disclosures:
Lawrence Zhou, MD1, Aastha V. Bharwad, MD2, Daly Al-Hadeethi, MD2, Rahul Shekhar, MD2, Andrew Osbeck, PA-C2, William Palko, MD3, Kyle Rowe, MD4, William J. Salyers, MD, MPH2. P3245 - Gut Instincts: Navigating a Hidden Case of Gastrointestinal Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1The University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine, Wichita, KS; 3Wesley Medical Center, Wichita, KS; 4University of Kansas Medical Center, Wichita, KS
Introduction: Amyloidosis encompasses disorders characterized by the misfolding and deposition of insoluble fibrils within organs causing dysfunction. GI involvement occurs in approximately 3% of cases, and overall less than 1% later also develop multiple myeloma (MM). Clinical manifestations are usually nonspecific such as chronic diarrhea, weight loss, abdominal pain, and bloating. We present a case of GI amyloidosis in the absence of MM.
Case Description/Methods: A 61 year-old female with history of familial adenomatous polyposis status-post colectomy with ileostomy, and chronically high alkaline phosphatase (ALP) was admitted with diarrhea, dehydration and kidney injury. Labs were also significant for aspartate aminotransferase 75 U/L, alanine aminotransferase 117 U/L, ALP 1304 U/L, and gamma-glutamyl transpeptidase (GGT) 1174 U/L. Prior hepatitis workup was negative, and magnetic resonance cholangiopancreatography showed intra- and extrahepatic biliary dilatation and lack of smooth tapering, so outpatient liver biopsy was planned. Endoscopy was performed due to profuse diarrhea and biopsies showed a micro-globular pattern of amyloid deposition within the lamina propria and submucosa (Figure A-D).
Prior to following up on the findings of gastrointestinal amyloidosis, the patient was admitted for acute renal failure. Free light chains were elevated, but protein electrophoresis and serologies were negative. She was started on prednisone for suspected nephrotic syndrome and biopsy revealed light chain (AL) amyloidosis. ALP and GGT peaked at 4259 U/L and 1547 U/L respectively. She subsequently started hemodialysis.
Before she could see oncology, she was admitted for life-threatening hyperkalemia after missing dialysis. She was started on cyclophosphamide, bortezomib, and dexamethasone (CyBorD), but developed severe methicillin-resistant Staphylococcus aureus (MRSA) bacteremia and empyema leading to intubation. Unfortunately, she continued to decompensate and was ultimately placed on hospice.
Discussion: Intestinal involvement is rare, occurring typically as part of systemic amyloidosis. Hepatic amyloidosis should be suspected in patients with weight loss or hepatomegaly, along with elevated ALP, proteinuria, and signs of hyposplenism, but requires biopsy confirmation. This patient’s disease progressed to renal failure and was complicated by hyposplenism manifesting as MRSA infection. Although no therapies are approved for AL amyloidosis, CYBorD regimen is the standard treatment.
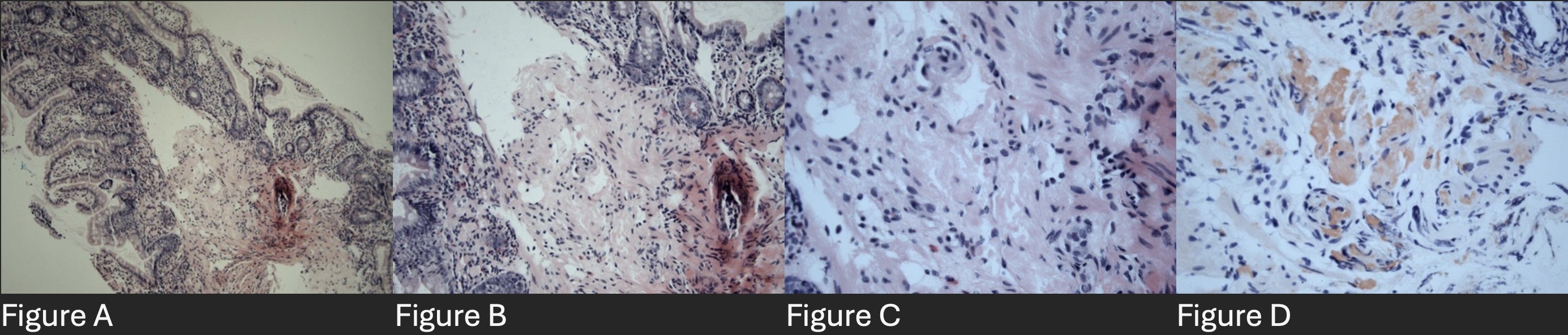
Figure: Figure A - Neo terminal ileum H&E 10X. Figure B - Neo terminal ileum H&E 20X. Figure C - Neo terminal ileum H&E 40X. Figure D - Neo terminal ileum Congo Red Stain 40X.
Disclosures:
Lawrence Zhou indicated no relevant financial relationships.
Aastha Bharwad indicated no relevant financial relationships.
Daly Al-Hadeethi indicated no relevant financial relationships.
Rahul Shekhar indicated no relevant financial relationships.
Andrew Osbeck indicated no relevant financial relationships.
William Palko indicated no relevant financial relationships.
Kyle Rowe indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Lawrence Zhou, MD1, Aastha V. Bharwad, MD2, Daly Al-Hadeethi, MD2, Rahul Shekhar, MD2, Andrew Osbeck, PA-C2, William Palko, MD3, Kyle Rowe, MD4, William J. Salyers, MD, MPH2. P3245 - Gut Instincts: Navigating a Hidden Case of Gastrointestinal Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
