Monday Poster Session
Category: Small Intestine
P3247 - A Rare Case of Duodenal Adenocarcinoma in a 22-Year-Old
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ahmun Zafar, DO
Mount Sinai West, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Ahmun Zafar, DO, Alexandria Markley, MD, Allison Wang, MD, Mohamed Rabie, MD, Bruce P. Gelman, MD
Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Duodenal adenocarcinoma is rare, accounting for less than 1% of all gastrointestinal malignancies. Diagnosis is often delayed until symptoms such as abdominal pain, nausea, vomiting, and weight loss are present. Anemia, obstruction, and jaundice are associated with advanced disease. We present a case of duodenal adenocarcinoma.
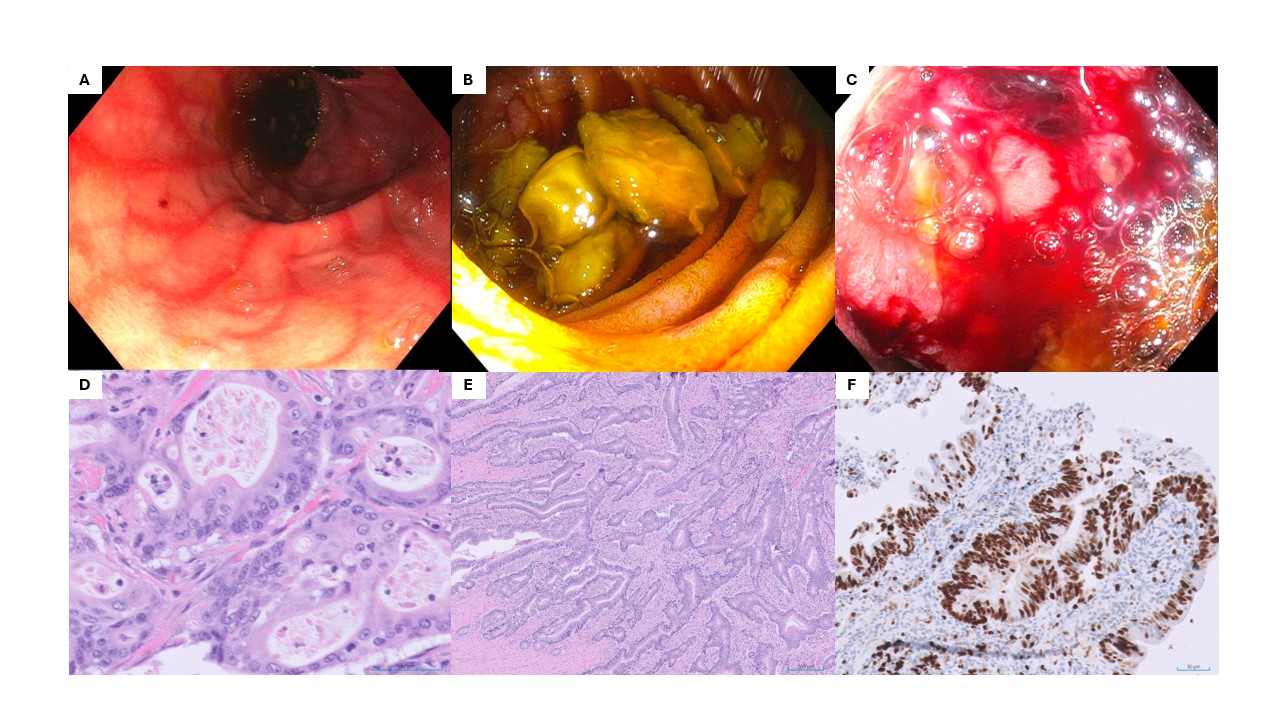
Case Description/Methods: A 22-year-old female with no past medical history presented with two weeks of epigastric pain and one day of nausea and vomiting. Physical exam revealed epigastric tenderness. An abdominal computed tomography (CT) scan revealed a 4.2x4.3 cm soft tissue mass at the distal duodenum, causing proximal duodenal and stomach distention. Esophagogastroduodenoscopy (EGD) showed an ulcerated, friable mass in the third portion of the duodenum. Pathology confirmed moderately differentiated invasive adenocarcinoma arising from a small intestinal adenoma with high-grade dysplasia. Tumor marker CA19-9 was 38.6 and chest CT showed no metastases. She underwent a small bowel resection with duodenojejunostomy and resection of eight lymph nodes. Postoperative pathology confirmed invasive adenocarcinoma, moderately differentiated, invading the subserosa, with clean surgical margins and negative lymph nodes. Immunohistochemical testing revealed intact DNA mismatch repair proteins, suggesting a low likelihood of microsatellite instability or Lynch syndrome. Following discharge, she had two negative circulating tumor DNA (ctDNA) tests and abdominal CT showed no recurrent mass or significant adenopathy. She was offered six months of capecitabine because she had eight lymph nodes, instead of 12, removed. She stopped after five weeks due to nausea and skin darkening. A second ctDNA test was negative. She was referred to genetic counseling, but further testing has not yet been completed.
Discussion: Genetics, high-fat diet, smoking, and inflammatory bowel diseases have been proposed as risk factors for duodenal adenocarcinoma. Our patient had no identifiable risk factors. Diagnosis is made using endoscopy, imaging, and histology. Characteristic EGD findings include mucosal ulceration, visible mass, and stenosis or obstruction. Histologic findings include cellular atypia, glandular architecture, and nuclear pleomorphism. Imaging typically reveals a localized soft tissue mass, duodenal wall thickening, or narrowing of bowel. Surgical resection is the primary treatment. Chemotherapy and radiation are offered in advanced disease or if there is a high risk of recurrence.
Disclosures:
Ahmun Zafar, DO, Alexandria Markley, MD, Allison Wang, MD, Mohamed Rabie, MD, Bruce P. Gelman, MD. P3247 - A Rare Case of Duodenal Adenocarcinoma in a 22-Year-Old, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mount Sinai West, Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Duodenal adenocarcinoma is rare, accounting for less than 1% of all gastrointestinal malignancies. Diagnosis is often delayed until symptoms such as abdominal pain, nausea, vomiting, and weight loss are present. Anemia, obstruction, and jaundice are associated with advanced disease. We present a case of duodenal adenocarcinoma.
Case Description/Methods: A 22-year-old female with no past medical history presented with two weeks of epigastric pain and one day of nausea and vomiting. Physical exam revealed epigastric tenderness. An abdominal computed tomography (CT) scan revealed a 4.2x4.3 cm soft tissue mass at the distal duodenum, causing proximal duodenal and stomach distention. Esophagogastroduodenoscopy (EGD) showed an ulcerated, friable mass in the third portion of the duodenum. Pathology confirmed moderately differentiated invasive adenocarcinoma arising from a small intestinal adenoma with high-grade dysplasia. Tumor marker CA19-9 was 38.6 and chest CT showed no metastases. She underwent a small bowel resection with duodenojejunostomy and resection of eight lymph nodes. Postoperative pathology confirmed invasive adenocarcinoma, moderately differentiated, invading the subserosa, with clean surgical margins and negative lymph nodes. Immunohistochemical testing revealed intact DNA mismatch repair proteins, suggesting a low likelihood of microsatellite instability or Lynch syndrome. Following discharge, she had two negative circulating tumor DNA (ctDNA) tests and abdominal CT showed no recurrent mass or significant adenopathy. She was offered six months of capecitabine because she had eight lymph nodes, instead of 12, removed. She stopped after five weeks due to nausea and skin darkening. A second ctDNA test was negative. She was referred to genetic counseling, but further testing has not yet been completed.
Discussion: Genetics, high-fat diet, smoking, and inflammatory bowel diseases have been proposed as risk factors for duodenal adenocarcinoma. Our patient had no identifiable risk factors. Diagnosis is made using endoscopy, imaging, and histology. Characteristic EGD findings include mucosal ulceration, visible mass, and stenosis or obstruction. Histologic findings include cellular atypia, glandular architecture, and nuclear pleomorphism. Imaging typically reveals a localized soft tissue mass, duodenal wall thickening, or narrowing of bowel. Surgical resection is the primary treatment. Chemotherapy and radiation are offered in advanced disease or if there is a high risk of recurrence.
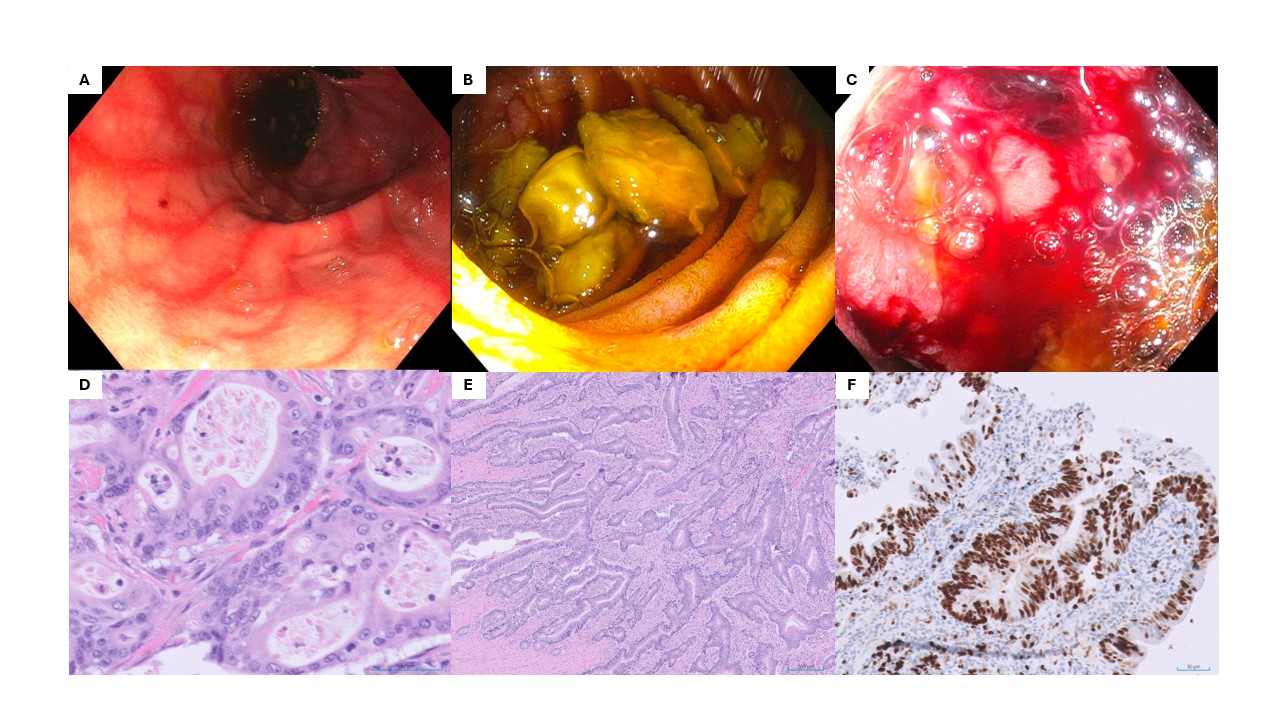
Figure: A. Endoscopy of gastric body – streaky gastritis. B. Endoscopy of third portion of the duodenum with solid food residue. C. Endoscopy of third portion of the duodenum – stenosis s/p multiple biopsies. D. Pathology: high power field of malignant glands with dysplastic cells showing loss of orientation, enlarged and irregular nuclei, and prominent nucleoli. E. Pathology: low power field on slide from resection specimen showing invasive moderately differentiating adenocarcinoma invading the submucosa. F. Pathology: proliferative index Ki67 shows ~60% staining on one of the malignant invasive glands indicating high rate of cell proliferation.
Disclosures:
Ahmun Zafar indicated no relevant financial relationships.
Alexandria Markley indicated no relevant financial relationships.
Allison Wang indicated no relevant financial relationships.
Mohamed Rabie indicated no relevant financial relationships.
Bruce Gelman indicated no relevant financial relationships.
Ahmun Zafar, DO, Alexandria Markley, MD, Allison Wang, MD, Mohamed Rabie, MD, Bruce P. Gelman, MD. P3247 - A Rare Case of Duodenal Adenocarcinoma in a 22-Year-Old, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
