Monday Poster Session
Category: Small Intestine
P3252 - Patent Stent, Wrong Lumen: A Rare Case of Duodenal Perforation Secondary to an Inferior Vena Cava Stent
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Iqra Kazi, MD
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Iqra Kazi, MD1, Sushreyta Rose, DO2, Jaya Vasudevan, MD3, Randy Wright, MD1
1University of Texas Health San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX
Introduction: Endovenous stenting of the inferior vena cava (IVC) has emerged as a safe, minimally invasive method to treat veno-occlusive disease. Although IVC filters carry known complications of duodenal perforation and duodeno-caval fistulas, similar complications with IVC stents have not been reported in the literature. We present a case of an IVC stent placed for venous thromboembolic disease causing perforation of the duodenum.
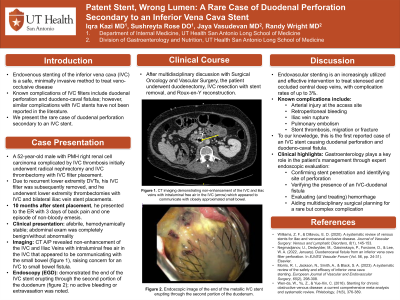
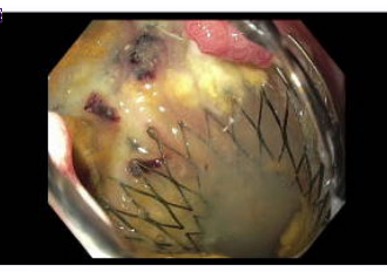
Case Description/Methods: A 52-year-old male with PMH of R renal cell carcinoma complicated by IVC thrombosis underwent radical nephrectomy and IVC thrombectomy with IVC filter placement. Due to recurrent lower extremity DVTs, his IVC filter was removed, and lower extremity thrombectomy with IVC and bilateral iliac vein stent placements were performed. Ten months later, the patient presented to the ER with 3 days of back pain and one episode of non-bloody emesis. On presentation, he was afebrile, hemodynamically stable, with a benign abdominal exam. Computerized Tomography of the Abdomen/Pelvis revealed non-enhancement of the IVC and iliac veins with significant intraluminal free air in the IVC which appeared to communicate with closely approximated small bowel- raising concern for an IVC to small bowel fistula. GI was consulted for endoscopic evaluation of these CT findings. On EGD, the end of a displaced metal IVC stent was seen erupting through the wall of the second portion of the duodenum without bleeding (figure 1); no endoscopic interventions were performed. After multidisciplinary discussion with Surgical Oncology and Vascular Surgery, the patient underwent duodenectomy, IVC resection with stent removal, and Roux-en-Y reconstruction.
Discussion: Endovascular stenting is an increasingly utilized and effective intervention to treat stenosed and occluded central deep veins, with complication rates of 3%. Complications include arterial injury at the access site, retroperitoneal bleeding, iliac vein rupture, pulmonary embolism, and stent thrombosis, migration or fracture. To our knowledge, this is the first reported case of an IVC stent causing duodenal perforation and duodeno-caval fistula. Gastroenterology may offer valuable input in patients with suspected duodenal perforation by IVC stents through endoscopic evaluation of the small bowel, by confirming stent penetration, identifying the site of perforation and fistula formation, and evaluating for hemorrhage- which in turn may aid in multidisciplinary surgical planning in the management of a rare but complex complication.
Disclosures:
Iqra Kazi, MD1, Sushreyta Rose, DO2, Jaya Vasudevan, MD3, Randy Wright, MD1. P3252 - Patent Stent, Wrong Lumen: A Rare Case of Duodenal Perforation Secondary to an Inferior Vena Cava Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health San Antonio, San Antonio, TX; 2UTHSCSA, San Antonio, TX; 3University of Texas Health Science Center, San Antonio, TX
Introduction: Endovenous stenting of the inferior vena cava (IVC) has emerged as a safe, minimally invasive method to treat veno-occlusive disease. Although IVC filters carry known complications of duodenal perforation and duodeno-caval fistulas, similar complications with IVC stents have not been reported in the literature. We present a case of an IVC stent placed for venous thromboembolic disease causing perforation of the duodenum.
Case Description/Methods: A 52-year-old male with PMH of R renal cell carcinoma complicated by IVC thrombosis underwent radical nephrectomy and IVC thrombectomy with IVC filter placement. Due to recurrent lower extremity DVTs, his IVC filter was removed, and lower extremity thrombectomy with IVC and bilateral iliac vein stent placements were performed. Ten months later, the patient presented to the ER with 3 days of back pain and one episode of non-bloody emesis. On presentation, he was afebrile, hemodynamically stable, with a benign abdominal exam. Computerized Tomography of the Abdomen/Pelvis revealed non-enhancement of the IVC and iliac veins with significant intraluminal free air in the IVC which appeared to communicate with closely approximated small bowel- raising concern for an IVC to small bowel fistula. GI was consulted for endoscopic evaluation of these CT findings. On EGD, the end of a displaced metal IVC stent was seen erupting through the wall of the second portion of the duodenum without bleeding (figure 1); no endoscopic interventions were performed. After multidisciplinary discussion with Surgical Oncology and Vascular Surgery, the patient underwent duodenectomy, IVC resection with stent removal, and Roux-en-Y reconstruction.
Discussion: Endovascular stenting is an increasingly utilized and effective intervention to treat stenosed and occluded central deep veins, with complication rates of 3%. Complications include arterial injury at the access site, retroperitoneal bleeding, iliac vein rupture, pulmonary embolism, and stent thrombosis, migration or fracture. To our knowledge, this is the first reported case of an IVC stent causing duodenal perforation and duodeno-caval fistula. Gastroenterology may offer valuable input in patients with suspected duodenal perforation by IVC stents through endoscopic evaluation of the small bowel, by confirming stent penetration, identifying the site of perforation and fistula formation, and evaluating for hemorrhage- which in turn may aid in multidisciplinary surgical planning in the management of a rare but complex complication.
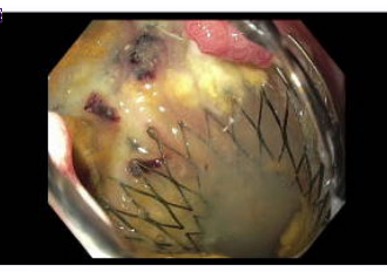
Figure: Figure 1. Endoscopic image of the end of the metallic IVC stent erupting through the second portion of the duodenum; no active bleeding or extravasation was noted.
Disclosures:
Iqra Kazi indicated no relevant financial relationships.
Sushreyta Rose indicated no relevant financial relationships.
Jaya Vasudevan indicated no relevant financial relationships.
Randy Wright indicated no relevant financial relationships.
Iqra Kazi, MD1, Sushreyta Rose, DO2, Jaya Vasudevan, MD3, Randy Wright, MD1. P3252 - Patent Stent, Wrong Lumen: A Rare Case of Duodenal Perforation Secondary to an Inferior Vena Cava Stent, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

