Monday Poster Session
Category: Small Intestine
P3257 - Ascites Indicative of Non-Cirrhotic Portal Hypertension Associated With Celiac Disease: A Case Report
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shuji Mitsuhashi, MBBS
Mayo Clinic
Rochester, MN
Presenting Author(s)
Shuji Mitsuhashi, MBBS, Yuan Yao, MD, Yi Zhu, MD, PhD, Christopher Dinh, MD, Don C.. Codipilly, MD, Joseph Murray, MD
Mayo Clinic, Rochester, MN
Introduction: Celiac disease (CD) is a chronic T-cell-mediated enteropathy triggered by gluten, affecting various organs beyond the gastrointestinal (GI) tract. We describe a case of CD complicated by ascites indicative of non-cirrhotic portal hypertension (PHT).
Case Description/Methods: A 35-year-old Caucasian male sought a second opinion of chronic diarrhea and progressive weight loss over two years. Initially diagnosed with a well-differentiated neuroendocrine tumor of the appendix, he underwent appendectomy and right hemicolectomy. Despite surgery, his symptoms worsened, with an 80 lb weight loss, muscle wasting, leg and scrotal swelling, abdominal distension, and increased bowel movements. He had no prior GI or liver disease, minimal alcohol intake, and no smoking or drug use. Family history included pancreatic cancer and primary biliary cholangitis.
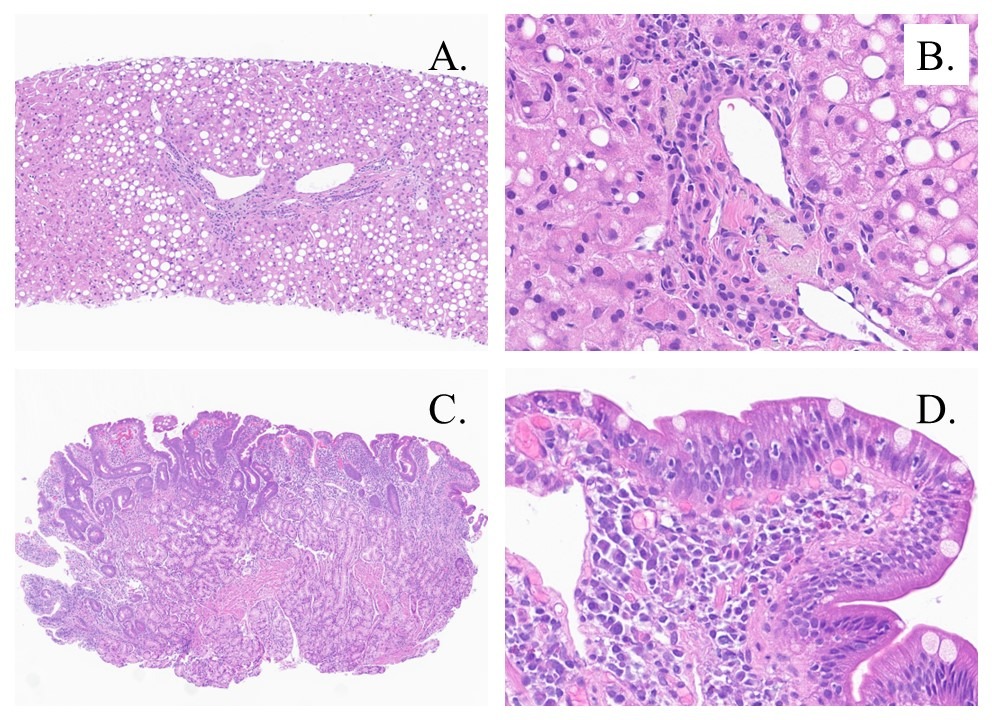
Workup revealed mildly elevated liver enzymes (ALT 166, AST 25, ALP 112), normal platelet, and low albumin (2.6 g/dl) suggested liver involvement, along with ascitic fluid indicating PHT. Echocardiogram ruled out heart failure or valvular disease; liver ultrasound with doppler confirmed patent hepatic vasculature and portal vein. Liver biopsy revealed moderate macrovesicular steatosis without fibrosis or cirrhosis, while duodenal biopsy indicated focal partial villous atrophy, crypt hyperplasia, and chronic inflammation (Fig 1). Positive celiac serologies and HLA DQ2/5 further supported celiac disease as the underlying pathology. Initiation of a strict gluten-free diet (GFD) led to significant improvement, resolving ascites, and normalization of lab results, including negative celiac serology, within six months.
Discussion: This case highlights an atypical presentation of CD with ascites in the absence of cirrhosis. Ascites in CD is rare, typically presenting with a low serum-ascites albumin gradient and variable protein content due to hypoalbuminemia from malabsorption or protein-losing enteropathy. However, CD can be associated with non-cirrhotic PHT. In this case, the underlying mechanism may involve increased intestinal permeability, chronic inflammation, and subsequent hypercoagulability affecting portal circulation. Importantly, the resolution of ascites and normalization of liver enzymes were achieved with a strict GFD, emphasizing the need for careful monitoring and comprehensive care in managing CD patients, especially encountering uncommon manifestations like ascites and hepatic involvement.
Disclosures:
Shuji Mitsuhashi, MBBS, Yuan Yao, MD, Yi Zhu, MD, PhD, Christopher Dinh, MD, Don C.. Codipilly, MD, Joseph Murray, MD. P3257 - Ascites Indicative of Non-Cirrhotic Portal Hypertension Associated With Celiac Disease: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Celiac disease (CD) is a chronic T-cell-mediated enteropathy triggered by gluten, affecting various organs beyond the gastrointestinal (GI) tract. We describe a case of CD complicated by ascites indicative of non-cirrhotic portal hypertension (PHT).
Case Description/Methods: A 35-year-old Caucasian male sought a second opinion of chronic diarrhea and progressive weight loss over two years. Initially diagnosed with a well-differentiated neuroendocrine tumor of the appendix, he underwent appendectomy and right hemicolectomy. Despite surgery, his symptoms worsened, with an 80 lb weight loss, muscle wasting, leg and scrotal swelling, abdominal distension, and increased bowel movements. He had no prior GI or liver disease, minimal alcohol intake, and no smoking or drug use. Family history included pancreatic cancer and primary biliary cholangitis.
Workup revealed mildly elevated liver enzymes (ALT 166, AST 25, ALP 112), normal platelet, and low albumin (2.6 g/dl) suggested liver involvement, along with ascitic fluid indicating PHT. Echocardiogram ruled out heart failure or valvular disease; liver ultrasound with doppler confirmed patent hepatic vasculature and portal vein. Liver biopsy revealed moderate macrovesicular steatosis without fibrosis or cirrhosis, while duodenal biopsy indicated focal partial villous atrophy, crypt hyperplasia, and chronic inflammation (Fig 1). Positive celiac serologies and HLA DQ2/5 further supported celiac disease as the underlying pathology. Initiation of a strict gluten-free diet (GFD) led to significant improvement, resolving ascites, and normalization of lab results, including negative celiac serology, within six months.
Discussion: This case highlights an atypical presentation of CD with ascites in the absence of cirrhosis. Ascites in CD is rare, typically presenting with a low serum-ascites albumin gradient and variable protein content due to hypoalbuminemia from malabsorption or protein-losing enteropathy. However, CD can be associated with non-cirrhotic PHT. In this case, the underlying mechanism may involve increased intestinal permeability, chronic inflammation, and subsequent hypercoagulability affecting portal circulation. Importantly, the resolution of ascites and normalization of liver enzymes were achieved with a strict GFD, emphasizing the need for careful monitoring and comprehensive care in managing CD patients, especially encountering uncommon manifestations like ascites and hepatic involvement.
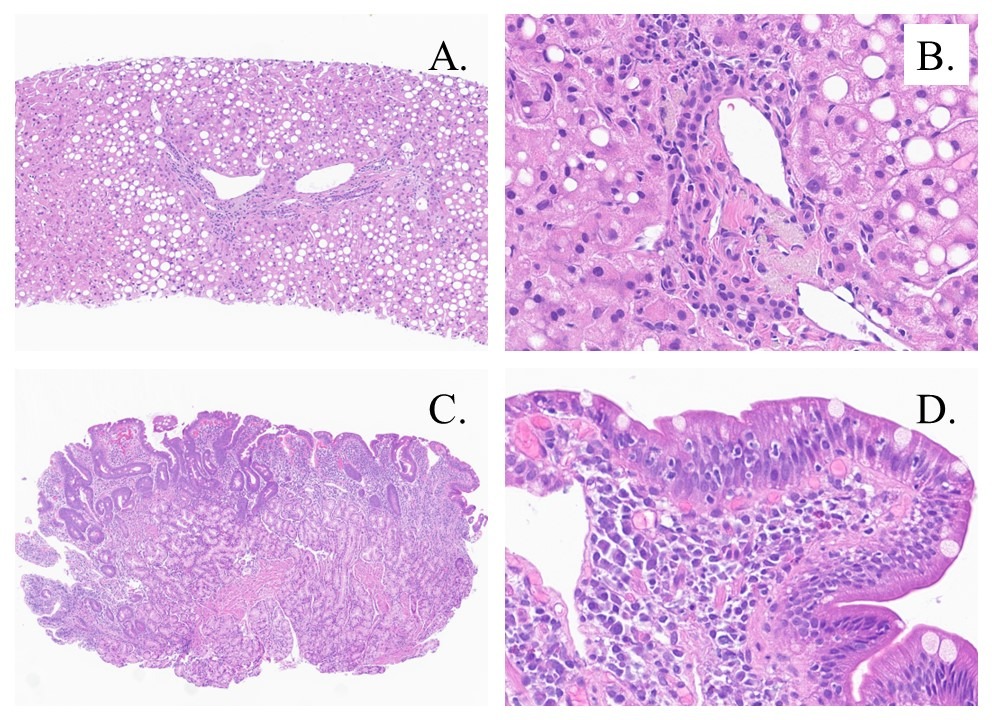
Figure: Figure 1. (A) Liver biopsy: Lower power (10x) view showing liver parenchyma with moderate macrovesicular steatosis, primarily involving zone 1 and zone 2, without significant lobular inflammation, Mallory hyaline, or ballooned cells. (B) Liver biopsy: High power (40x) view revealing prominent ceroid macrophages, consistent with resolving hepatitis. (C) Duodenal biopsy: Lower power (5x) view showing focal partial villous atrophy, crypt hyperplasia, and chronic inflammation. (D) Duodenal biopsy: High power (40x) view showing marked chronic inflammation and focal mild intraepithelial lymphocytosis.
Disclosures:
Shuji Mitsuhashi indicated no relevant financial relationships.
Yuan Yao indicated no relevant financial relationships.
Yi Zhu indicated no relevant financial relationships.
Christopher Dinh indicated no relevant financial relationships.
Don Codipilly indicated no relevant financial relationships.
Joseph Murray indicated no relevant financial relationships.
Shuji Mitsuhashi, MBBS, Yuan Yao, MD, Yi Zhu, MD, PhD, Christopher Dinh, MD, Don C.. Codipilly, MD, Joseph Murray, MD. P3257 - Ascites Indicative of Non-Cirrhotic Portal Hypertension Associated With Celiac Disease: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
