Monday Poster Session
Category: Small Intestine
P3264 - A Challenging Diagnosis of Low-grade Appendiceal Mucinous Neoplasm Mimicking Ovarian Cancer and Primary Biliary Cholangitis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- TL
Tooba Laeeq, MD
University of Nevada
Las Vegas, NV
Presenting Author(s)
Tooba Laeeq, MD1, Kyaw Min Tun, DO2, Adam Khattak, DO3, Ali Kia, MD3
1University of Nevada, Las Vegas, NV; 2Creighton University School of Medicine, Las Vegas, NV; 3Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV
Introduction: Low-grade appendiceal mucinous tumors (LAMNs) are a rare type of appendiceal tumor, often incidentally found without infiltrative growth. We present a case of LAMN presenting with acute kidney injury, elevated liver markers, and ascites.
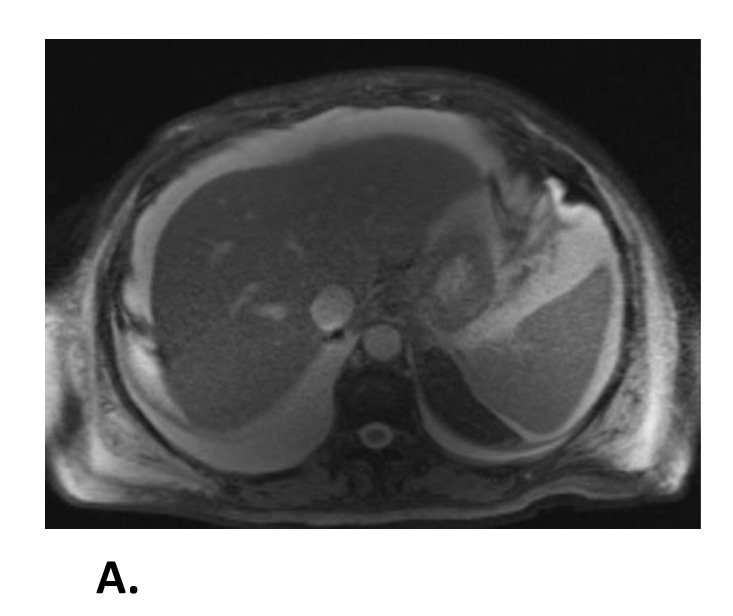
Case Description/Methods: A 72 year-old female with no known history presented with worsening abdominal distension for two weeks. Physical exam confirmed a distended abdomen. Labs showed WBC 12.8 k/mm3, lactic acid 2.4 mmol/l, creatinine 5.43 mg/dl (baseline 0.7 mg/dl), AST 120 iu/l, ALT 58 u/l, alkaline phosphatase 468 u/l, and total bilirubin 6.7 mg/dl. Imaging revealed moderate ascites with nodular liver. Paracentesis labs, anti-mitochondrial antibody, anti-smooth muscle antibody, and a liver biopsy were inconclusive. Further workup with a renal biopsy and autoimmune panel were unremarkable. However, CA-125 and CA 19-9 levels were elevated at 1279 u/ml and 95 u/ml, respectively, raising concern for ovarian malignancy. The abnormally thickened endometrial lining was noted on transvaginal ultrasound. A hysterectomy with bilateral oophorectomy and appendectomy was subsequently performed. Histology from the appendix revealed an intact appendix wall with mucinous proliferation suggestive of low-grade appendiceal mucinous neoplasm. Due to the patient’s stability, she was discharged and received outpatient care with gastroenterology for colonoscopy and oncology.
Discussion: LAMNs remain poorly understood and are found in only 0.2-0.3% of the appendectomy specimens. Diagnosis is often incidental and made histopathologically. Treatment of LAMNs varies from a radical appendectomy in patients with in-situ disease to ileocecal resection with hyperthermic intraperitoneal chemotherapy or cytoreductive therapy for pseudomyxoma peritonei (PMP). Unfortunately, PMP has a recurrence rate of 3%. Some data suggests that in the absence of PMP, a CT scan of the abdomen is recommended every six months postoperatively, followed by yearly for four years and biennially for six more years, along with tumor markers (CEA, CA19-9, and CA125). Additionally, colorectal cancer should be excluded with a colonoscopy in these patients due to the associated risks.
Disclosures:
Tooba Laeeq, MD1, Kyaw Min Tun, DO2, Adam Khattak, DO3, Ali Kia, MD3. P3264 - A Challenging Diagnosis of Low-grade Appendiceal Mucinous Neoplasm Mimicking Ovarian Cancer and Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Nevada, Las Vegas, NV; 2Creighton University School of Medicine, Las Vegas, NV; 3Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, NV
Introduction: Low-grade appendiceal mucinous tumors (LAMNs) are a rare type of appendiceal tumor, often incidentally found without infiltrative growth. We present a case of LAMN presenting with acute kidney injury, elevated liver markers, and ascites.
Case Description/Methods: A 72 year-old female with no known history presented with worsening abdominal distension for two weeks. Physical exam confirmed a distended abdomen. Labs showed WBC 12.8 k/mm3, lactic acid 2.4 mmol/l, creatinine 5.43 mg/dl (baseline 0.7 mg/dl), AST 120 iu/l, ALT 58 u/l, alkaline phosphatase 468 u/l, and total bilirubin 6.7 mg/dl. Imaging revealed moderate ascites with nodular liver. Paracentesis labs, anti-mitochondrial antibody, anti-smooth muscle antibody, and a liver biopsy were inconclusive. Further workup with a renal biopsy and autoimmune panel were unremarkable. However, CA-125 and CA 19-9 levels were elevated at 1279 u/ml and 95 u/ml, respectively, raising concern for ovarian malignancy. The abnormally thickened endometrial lining was noted on transvaginal ultrasound. A hysterectomy with bilateral oophorectomy and appendectomy was subsequently performed. Histology from the appendix revealed an intact appendix wall with mucinous proliferation suggestive of low-grade appendiceal mucinous neoplasm. Due to the patient’s stability, she was discharged and received outpatient care with gastroenterology for colonoscopy and oncology.
Discussion: LAMNs remain poorly understood and are found in only 0.2-0.3% of the appendectomy specimens. Diagnosis is often incidental and made histopathologically. Treatment of LAMNs varies from a radical appendectomy in patients with in-situ disease to ileocecal resection with hyperthermic intraperitoneal chemotherapy or cytoreductive therapy for pseudomyxoma peritonei (PMP). Unfortunately, PMP has a recurrence rate of 3%. Some data suggests that in the absence of PMP, a CT scan of the abdomen is recommended every six months postoperatively, followed by yearly for four years and biennially for six more years, along with tumor markers (CEA, CA19-9, and CA125). Additionally, colorectal cancer should be excluded with a colonoscopy in these patients due to the associated risks.
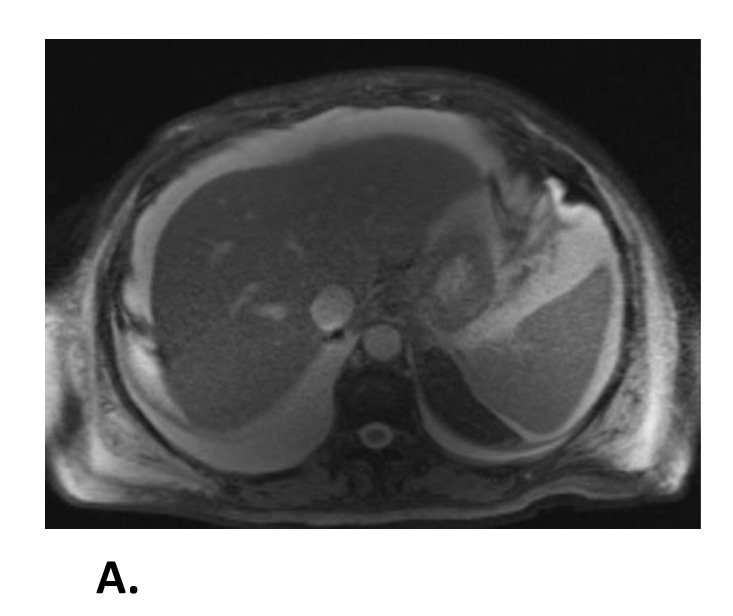
Figure: A. Magnetic Resonance Imaging of the Abdomen and Pelvis without contrast showing moderate to large amounts of abdominal ascites.
Disclosures:
Tooba Laeeq indicated no relevant financial relationships.
Kyaw Min Tun indicated no relevant financial relationships.
Adam Khattak indicated no relevant financial relationships.
Ali Kia indicated no relevant financial relationships.
Tooba Laeeq, MD1, Kyaw Min Tun, DO2, Adam Khattak, DO3, Ali Kia, MD3. P3264 - A Challenging Diagnosis of Low-grade Appendiceal Mucinous Neoplasm Mimicking Ovarian Cancer and Primary Biliary Cholangitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
