Monday Poster Session
Category: Small Intestine
P3294 - Post-Transplant Lymphoproliferative Disorder of the Small Bowel 13 Years After Kidney Transplant
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Christopher J. Varlamos, BS
Case Western Reserve University School of Medicine
Cleveland Heights, OH
Presenting Author(s)
Christopher J. Varlamos, BS1, Dayyan Adoor, MD2, Amy Hosmer, MD3
1Case Western Reserve University School of Medicine, Cleveland Heights, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 3University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Post-transplant lymphoproliferative disorder (PTLD) refers to lymphomas that occur as a consequence of chronic immunosuppression in hematopoietic stem cell or solid organ transplantation (SOT). Most PTLD cases are extranodal and occur within the first year of transplant. Though variable, PTLD most commonly presents with constitutional symptoms such as fever, malaise, night sweats, and fatigue. We present a unique case of PTLD manifesting with atypical symptoms 13 years post-SOT.
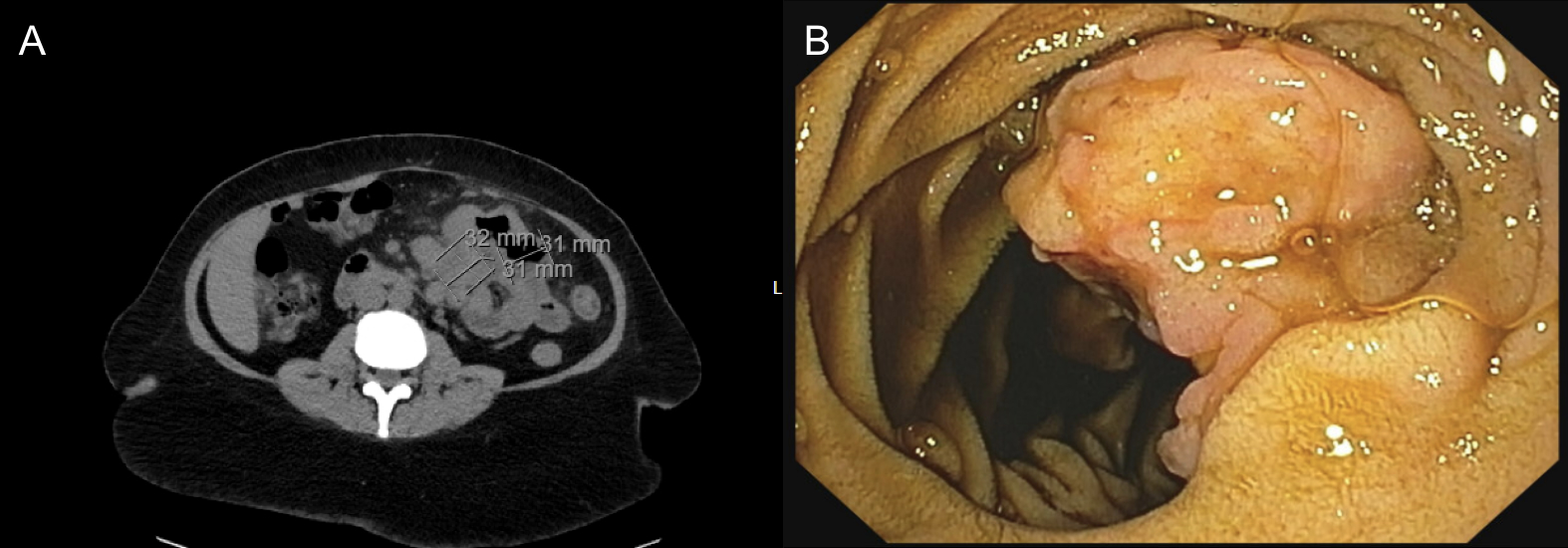
Case Description/Methods: A 47-year-old female with history of deceased donor kidney transplant 13 years prior presented with a 4-week history of abdominal pain and constipation. Initially attributed to gastroparesis due to recent Semaglutide initiation, her pain persisted and worsened in severity and frequency after medication discontinuation. Upper endoscopy and colonoscopy were unrevealing, but subsequent CT scan revealed enlarged masses within the mesentery and mesenteric and retroperitoneal lymphadenopathy (Figure A). She was referred for enteroscopy and endoscopic ultrasound for tissue sampling. Enteroscopy revealed a multilobular and ulcerated mass in the proximal jejunum (Figure B) and biopsy confirmed CD20+ diffuse large B-cell lymphoma. Prior to diagnosis, she had no changes in her immunosuppression regimen of Tacrolimus 8mg BID and Azathioprine 150mg daily. She received 8 infusions of Rituximab and a 5 day course of prednisone 50mg then transitioned to 5mg. Tacrolimus was reduced to 7mg BID and Azathioprine was discontinued. She continues to progress well with noted symptomatic and radiographic improvement since diagnosis.
Discussion: This case illustrates a deviation from the norm in PTLD presentation post-SOT. PTLD is a life-threatening complication and the most common malignancy complicating SOT. Most cases occur in the GI tract due to its higher concentration of B and T lymphocytes. However, incidence remains variable and depends on many factors including patient population, age < 10 or > 60 years, time post-transplant, allograft type, degree of immunosuppression, and EBV serostatus. While incidence over 5 years is estimated to be only 1.5% in kidney transplants, it has been reported to reach 33% in intestinal and multiorgan transplants. Thus, this case underscores the importance of maintaining a high index of suspicion for PTLD in atypical patients who are decades removed from transplant, lack classic risk factors such as age and allograft type, and present without characteristic constitutional symptoms.
Disclosures:
Christopher J. Varlamos, BS1, Dayyan Adoor, MD2, Amy Hosmer, MD3. P3294 - Post-Transplant Lymphoproliferative Disorder of the Small Bowel 13 Years After Kidney Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Case Western Reserve University School of Medicine, Cleveland Heights, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 3University of Pittsburgh Medical Center, Pittsburgh, PA
Introduction: Post-transplant lymphoproliferative disorder (PTLD) refers to lymphomas that occur as a consequence of chronic immunosuppression in hematopoietic stem cell or solid organ transplantation (SOT). Most PTLD cases are extranodal and occur within the first year of transplant. Though variable, PTLD most commonly presents with constitutional symptoms such as fever, malaise, night sweats, and fatigue. We present a unique case of PTLD manifesting with atypical symptoms 13 years post-SOT.
Case Description/Methods: A 47-year-old female with history of deceased donor kidney transplant 13 years prior presented with a 4-week history of abdominal pain and constipation. Initially attributed to gastroparesis due to recent Semaglutide initiation, her pain persisted and worsened in severity and frequency after medication discontinuation. Upper endoscopy and colonoscopy were unrevealing, but subsequent CT scan revealed enlarged masses within the mesentery and mesenteric and retroperitoneal lymphadenopathy (Figure A). She was referred for enteroscopy and endoscopic ultrasound for tissue sampling. Enteroscopy revealed a multilobular and ulcerated mass in the proximal jejunum (Figure B) and biopsy confirmed CD20+ diffuse large B-cell lymphoma. Prior to diagnosis, she had no changes in her immunosuppression regimen of Tacrolimus 8mg BID and Azathioprine 150mg daily. She received 8 infusions of Rituximab and a 5 day course of prednisone 50mg then transitioned to 5mg. Tacrolimus was reduced to 7mg BID and Azathioprine was discontinued. She continues to progress well with noted symptomatic and radiographic improvement since diagnosis.
Discussion: This case illustrates a deviation from the norm in PTLD presentation post-SOT. PTLD is a life-threatening complication and the most common malignancy complicating SOT. Most cases occur in the GI tract due to its higher concentration of B and T lymphocytes. However, incidence remains variable and depends on many factors including patient population, age < 10 or > 60 years, time post-transplant, allograft type, degree of immunosuppression, and EBV serostatus. While incidence over 5 years is estimated to be only 1.5% in kidney transplants, it has been reported to reach 33% in intestinal and multiorgan transplants. Thus, this case underscores the importance of maintaining a high index of suspicion for PTLD in atypical patients who are decades removed from transplant, lack classic risk factors such as age and allograft type, and present without characteristic constitutional symptoms.
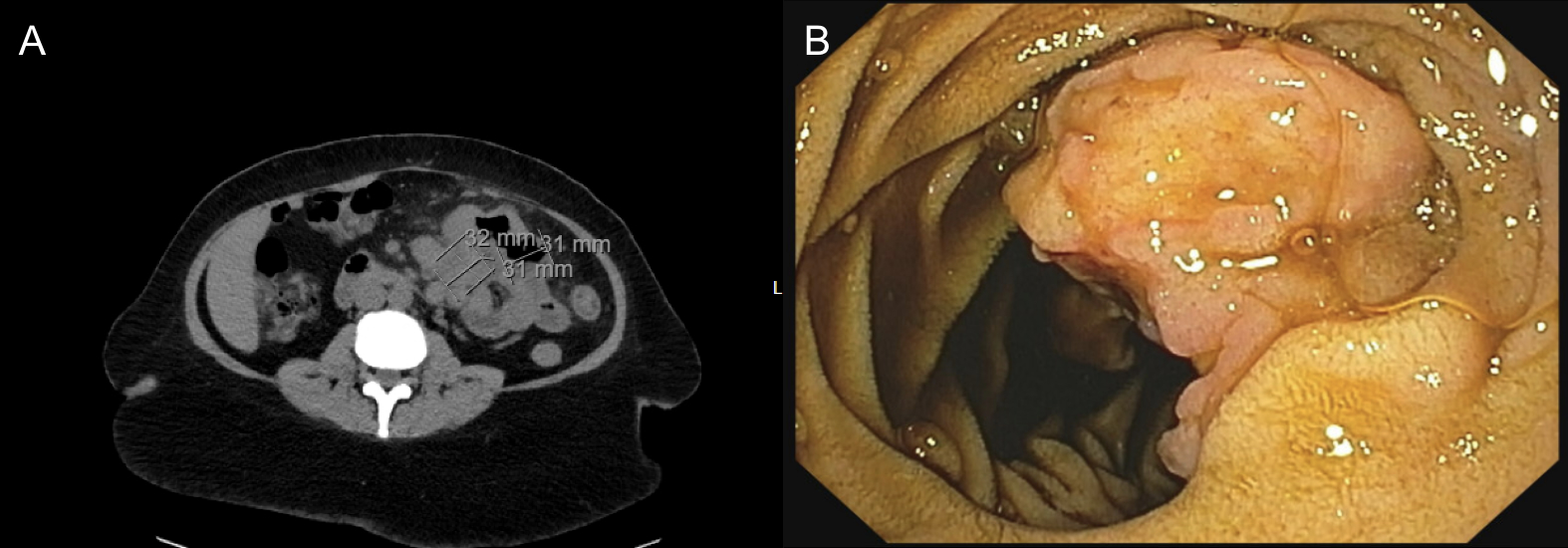
Figure: Figure A - CT abdomen; Figure B - Enteroscopy
Disclosures:
Christopher Varlamos indicated no relevant financial relationships.
Dayyan Adoor indicated no relevant financial relationships.
Amy Hosmer indicated no relevant financial relationships.
Christopher J. Varlamos, BS1, Dayyan Adoor, MD2, Amy Hosmer, MD3. P3294 - Post-Transplant Lymphoproliferative Disorder of the Small Bowel 13 Years After Kidney Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
