Monday Poster Session
Category: Stomach
P3317 - Examining the Risk of Developing Functional Dyspepsia Post-Helicobacter pylori Treatment: Insights From a Global Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- KK
Kaynat Khalid, DO
Case Western Reserve University / MetroHealth
Westlake, OH
Presenting Author(s)
Kaynat Khalid, DO1, Yan Sun, MD1, Gengqing Song, MD, PhD2
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Metrohealth Medical Center, Cleveland, OH
Introduction: Helicobacter pylori (H pylori) is one of the most prevalent bacterial infections worldwide, primarily affecting the stomach. Standard therapy for H. pylori infection involves a proton pump inhibitor (PPI) or potassium-competitive acid blocker (PCAB) combined with antibiotics like amoxicillin, clarithromycin, or metronidazole, and may include bismuth subsalicylate. We sought to assess the association between patients with H pylori infection post-treatment and the development of functional dyspepsia.
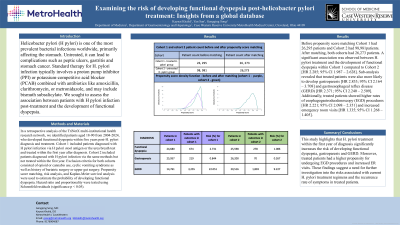
Methods: In a retrospective analysis of the TriNetX multi-institutional health research network, we identified patients aged 18-90 who developed functional dyspepsia within five years post-H. pylori diagnosis and treatment. Cohort 1 included patients diagnosed with H pylori infection via H pylori stool antigen or the urea breath test and treated within the first year after diagnosis. Cohort 2 included patients diagnosed with H pylori infection via the same methods but not treated within the first year. Exclusion criteria included opioid or cannabis use, cyclic vomiting syndrome and bariatric or upper gut surgery. Propensity score matching, risk analysis, and Kaplan-Meier survival analysis were used to estimate the probability of developing functional dyspepsia. Hazard ratio and proportionality were tested using Schoenfeld residuals (significance p< 0.05).
Results: Before propensity score matching Cohort 1 had 26,295 patients and Cohort 2 had 98,981patients. After matching, both cohorts had 26,273 patients. A significant association was observed between H. pylori treatment and the development of functional dyspepsia within Cohort 1 [HR 2.285; 95% CI 1.987–2.628]. Sub-analysis revealed that treated patients were more likely to develop gastroparesis [HR 2.833; 95% CI 2.164–3.708] and gastroesophageal reflux disease (GERD) [HR 2.371; 95% CI 2.240– 2.509]. Treated patients also showed higher rates of esophagogastroduodenoscopy (EGD) procedures [HR 2.221; 95% CI 2.098–2.351] and increased emergency room visits [HR 1.335; 95% CI 1.268–1.405].
Discussion: This study highlights that H. pylori treatment within the first year of diagnosis significantly increases the risk of developing functional dyspepsia, gastroparesis, and GERD. Treated patients had a higher propensity for undergoing EGD procedures and increased ER visits. These findings suggest a need for further investigation into the risks associated with current H. pylori treatment regimens and the recurrence rate of symptoms in treated patients.
Disclosures:
Kaynat Khalid, DO1, Yan Sun, MD1, Gengqing Song, MD, PhD2. P3317 - Examining the Risk of Developing Functional Dyspepsia Post-<i>Helicobacter pylori</i> Treatment: Insights From a Global Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Case Western Reserve University / MetroHealth, Cleveland, OH; 2Metrohealth Medical Center, Cleveland, OH
Introduction: Helicobacter pylori (H pylori) is one of the most prevalent bacterial infections worldwide, primarily affecting the stomach. Standard therapy for H. pylori infection involves a proton pump inhibitor (PPI) or potassium-competitive acid blocker (PCAB) combined with antibiotics like amoxicillin, clarithromycin, or metronidazole, and may include bismuth subsalicylate. We sought to assess the association between patients with H pylori infection post-treatment and the development of functional dyspepsia.
Methods: In a retrospective analysis of the TriNetX multi-institutional health research network, we identified patients aged 18-90 who developed functional dyspepsia within five years post-H. pylori diagnosis and treatment. Cohort 1 included patients diagnosed with H pylori infection via H pylori stool antigen or the urea breath test and treated within the first year after diagnosis. Cohort 2 included patients diagnosed with H pylori infection via the same methods but not treated within the first year. Exclusion criteria included opioid or cannabis use, cyclic vomiting syndrome and bariatric or upper gut surgery. Propensity score matching, risk analysis, and Kaplan-Meier survival analysis were used to estimate the probability of developing functional dyspepsia. Hazard ratio and proportionality were tested using Schoenfeld residuals (significance p< 0.05).
Results: Before propensity score matching Cohort 1 had 26,295 patients and Cohort 2 had 98,981patients. After matching, both cohorts had 26,273 patients. A significant association was observed between H. pylori treatment and the development of functional dyspepsia within Cohort 1 [HR 2.285; 95% CI 1.987–2.628]. Sub-analysis revealed that treated patients were more likely to develop gastroparesis [HR 2.833; 95% CI 2.164–3.708] and gastroesophageal reflux disease (GERD) [HR 2.371; 95% CI 2.240– 2.509]. Treated patients also showed higher rates of esophagogastroduodenoscopy (EGD) procedures [HR 2.221; 95% CI 2.098–2.351] and increased emergency room visits [HR 1.335; 95% CI 1.268–1.405].
Discussion: This study highlights that H. pylori treatment within the first year of diagnosis significantly increases the risk of developing functional dyspepsia, gastroparesis, and GERD. Treated patients had a higher propensity for undergoing EGD procedures and increased ER visits. These findings suggest a need for further investigation into the risks associated with current H. pylori treatment regimens and the recurrence rate of symptoms in treated patients.
Disclosures:
Kaynat Khalid indicated no relevant financial relationships.
Yan Sun indicated no relevant financial relationships.
Gengqing Song indicated no relevant financial relationships.
Kaynat Khalid, DO1, Yan Sun, MD1, Gengqing Song, MD, PhD2. P3317 - Examining the Risk of Developing Functional Dyspepsia Post-<i>Helicobacter pylori</i> Treatment: Insights From a Global Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
