Monday Poster Session
Category: Stomach
P3375 - Strongyloidiasis Causing Gastric Outlet Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Zachary Mitchell, MD
Atrium Health Wake Forest Baptist
Winston-Salem, NC
Presenting Author(s)
Zachary Mitchell, MD1, Jigisha Srivastav, MD2, Bryan Koppa, MD1
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest Baptist Health, Winston-Salem, NC
Introduction: Strongyloides stercoralis is a nematode that can cause a disseminated infection in individuals and can manifest as a variety of cutaneous, respiratory, and gastrointestinal symptoms. This case focuses on a rarely documented presentation of gastric outlet obstruction (GOO) secondary to strongyloides hyperinfection syndrome.
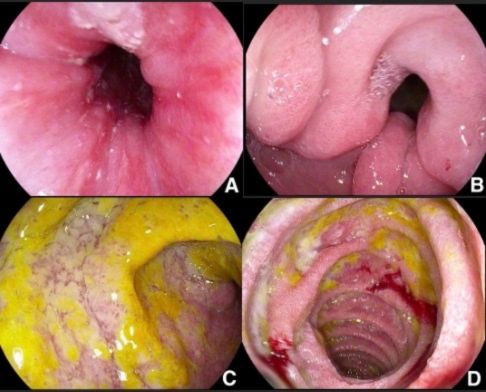
Case Description/Methods: A 71-year-old male with medical history significant for deceased donor renal transplant on immunosuppression presented with a two-day history of abdominal distention, nausea, non-bilious emesis, and poor oral intake. Patient had previously been admitted two days prior for similar complaints and was found to have dilated loops of bowel on abdominal XRAY. He was treated with nasogastric tube (NGT) with subsequent resolution of symptoms and therefore was discharged. On the second presentation, physical exam was notable for mild abdominal distention and diffuse abdominal tenderness, but normal bowel sounds. Abdominal XRAY revealed increased dilated loops of small bowel and stomach concerning for GOO. An NGT was placed with over three liters of coffee ground output in just over twelve hours. An upper endoscopy was performed which demonstrated severe grade D esophagitis, edematous mucosa and enlarged gastric folds, and severe generalized ulcerated mucosa throughout the entire duodenal bulb and parts of the duodenum. Biopsies of the prepyloric and duodenal mucosa were obtained and positive for Strongyloides. Of note, patient had a negative strongyloides IgG antibody before his transplant. The patient was started on subcutaneous Ivermectin due to concern for malabsorption in setting of paralytic ileus seen on computed tomography. Albendazole was also started per recommendations from infectious disease due to severe disease. On day three of admission, the patient’s clinical status decompensated and was escalated to the intensive care unit requiring intubation, vasopressors, and total parenteral nutrition. Unfortunately, the patient ultimately died due to complications from strongyloides hyperinfection syndrome.
Discussion: While strongyloidiasis is often an asymptomatic infection, immunocompromised patients can have rapid progression of life-threatening symptoms. Therefore, early recognition of symptoms is crucial due to the high mortality of strongyloides hyperinfection syndrome. This case highlights the importance of keeping strongyloides hyperinfection syndrome on the differential for immunocompromised patients who present with gastric outlet obstruction.
Disclosures:
Zachary Mitchell, MD1, Jigisha Srivastav, MD2, Bryan Koppa, MD1. P3375 - Strongyloidiasis Causing Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Atrium Health Wake Forest Baptist, Winston-Salem, NC; 2Wake Forest Baptist Health, Winston-Salem, NC
Introduction: Strongyloides stercoralis is a nematode that can cause a disseminated infection in individuals and can manifest as a variety of cutaneous, respiratory, and gastrointestinal symptoms. This case focuses on a rarely documented presentation of gastric outlet obstruction (GOO) secondary to strongyloides hyperinfection syndrome.
Case Description/Methods: A 71-year-old male with medical history significant for deceased donor renal transplant on immunosuppression presented with a two-day history of abdominal distention, nausea, non-bilious emesis, and poor oral intake. Patient had previously been admitted two days prior for similar complaints and was found to have dilated loops of bowel on abdominal XRAY. He was treated with nasogastric tube (NGT) with subsequent resolution of symptoms and therefore was discharged. On the second presentation, physical exam was notable for mild abdominal distention and diffuse abdominal tenderness, but normal bowel sounds. Abdominal XRAY revealed increased dilated loops of small bowel and stomach concerning for GOO. An NGT was placed with over three liters of coffee ground output in just over twelve hours. An upper endoscopy was performed which demonstrated severe grade D esophagitis, edematous mucosa and enlarged gastric folds, and severe generalized ulcerated mucosa throughout the entire duodenal bulb and parts of the duodenum. Biopsies of the prepyloric and duodenal mucosa were obtained and positive for Strongyloides. Of note, patient had a negative strongyloides IgG antibody before his transplant. The patient was started on subcutaneous Ivermectin due to concern for malabsorption in setting of paralytic ileus seen on computed tomography. Albendazole was also started per recommendations from infectious disease due to severe disease. On day three of admission, the patient’s clinical status decompensated and was escalated to the intensive care unit requiring intubation, vasopressors, and total parenteral nutrition. Unfortunately, the patient ultimately died due to complications from strongyloides hyperinfection syndrome.
Discussion: While strongyloidiasis is often an asymptomatic infection, immunocompromised patients can have rapid progression of life-threatening symptoms. Therefore, early recognition of symptoms is crucial due to the high mortality of strongyloides hyperinfection syndrome. This case highlights the importance of keeping strongyloides hyperinfection syndrome on the differential for immunocompromised patients who present with gastric outlet obstruction.
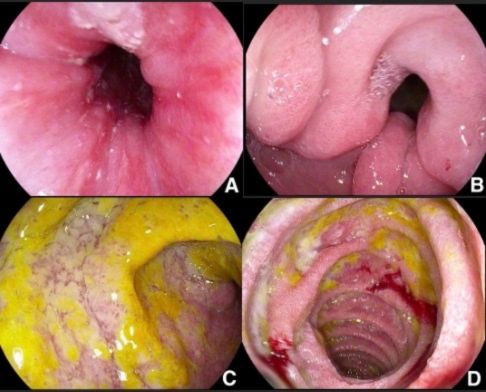
Figure: Fig 1A: Severe esophagitis present in the upper third of the esophagus. Fig 1B: Extensive edematous mucosa and enlarged gastric folds in the antrum. Fig 1C: Duodenal bulb ulceration. Fig 1D: Ulceration present in the second part of the duodenum.
Disclosures:
Zachary Mitchell indicated no relevant financial relationships.
Jigisha Srivastav indicated no relevant financial relationships.
Bryan Koppa indicated no relevant financial relationships.
Zachary Mitchell, MD1, Jigisha Srivastav, MD2, Bryan Koppa, MD1. P3375 - Strongyloidiasis Causing Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

