Monday Poster Session
Category: Stomach
P3376 - An Unusual Case of Isolated Gastric Amyloidosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Taras Halan, MD
Berkshire Medical Center
Pittsfield, MA
Presenting Author(s)
Taras Halan, MD1, Garrick H. Gu, MD2, Taylor Seacor, MD2, Mark Sterling, MD1, David Jones, MD3
1Berkshire Medical Center, Pittsfield, MA; 2University of Massachusetts, Worcester, MA; 3Berkshire Medical Center, Pittsifeld, MA
Introduction: Systemic amyloidosis, which can affect the gastrointestinal tract in 4% of cases, often manifests with diverse symptoms. While amyloid deposition commonly involves multiple organs, isolated gastric amyloidosis is rare, with an unclear etiology. Diagnostic challenges arise due to varied symptoms, leading to delayed identification. This case describes a 73-year-old female initially presenting with stroke-like symptoms, with an ultimate diagnosis of isolated gastric amyloidosis with discrete lesions.
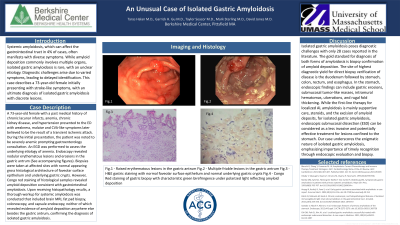
Case Description/Methods: A 73-year-old female with a past medical history of chronic lacunar infarcts, anemia, chronic kidney disease, and hypertension presented to the ED with weakness, malaise and CVA-like symptoms later believed to be the result of a transient ischemic attack. During the initial presentation, the patient was noted to be severely anemic prompting gastroenterology consultation. An EGD was performed to assess the underlying etiology of anemia. Endoscopy revealed nodular erythematous lesions and erosions in the gastric antrum (See accompanying figures). Biopsies were taken at affected sites with normal appearing gross histological architecture of foveolar surface epithelium and underlying gastric crypts. However, Congo red staining of histological samples revealed amyloid deposition consistent with gastrointestinal amyloidosis. Following biopsy confirmed diagnosis of amyloid in the GI tract, a thorough workup for systemic amyloidosis was conducted (Table 1).
Discussion: Isolated gastric amyloidosis poses diagnostic challenges with only 28 cases reported in the literature. The gold standard for diagnosis of both forms is biopsy confirmation of amyloid deposition. The site of highest diagnostic yield for direct biopsy verification of disease is the duodenum followed by stomach, colon, rectum and esophagus. In the stomach, endoscopic findings can include gastric erosions, submucosal tumor-like masses, intramural hematomas, ulcerations, and rugal fold thickening. While the first-line therapy for localized AL amyloidosis is mainly supportive care, steroids, and the excision of amyloid deposits, for isolated gastric amyloidosis, endoscopic submucosal dissection (ESD) can be considered as a less invasive and potentially effective treatment for lesions confined to the stomach. Our case underscores the enigmatic nature of isolated gastric amyloidosis, emphasizing timely recognition through endoscopic evaluation and biopsy.

Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Taras Halan, MD1, Garrick H. Gu, MD2, Taylor Seacor, MD2, Mark Sterling, MD1, David Jones, MD3. P3376 - An Unusual Case of Isolated Gastric Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Berkshire Medical Center, Pittsfield, MA; 2University of Massachusetts, Worcester, MA; 3Berkshire Medical Center, Pittsifeld, MA
Introduction: Systemic amyloidosis, which can affect the gastrointestinal tract in 4% of cases, often manifests with diverse symptoms. While amyloid deposition commonly involves multiple organs, isolated gastric amyloidosis is rare, with an unclear etiology. Diagnostic challenges arise due to varied symptoms, leading to delayed identification. This case describes a 73-year-old female initially presenting with stroke-like symptoms, with an ultimate diagnosis of isolated gastric amyloidosis with discrete lesions.
Case Description/Methods: A 73-year-old female with a past medical history of chronic lacunar infarcts, anemia, chronic kidney disease, and hypertension presented to the ED with weakness, malaise and CVA-like symptoms later believed to be the result of a transient ischemic attack. During the initial presentation, the patient was noted to be severely anemic prompting gastroenterology consultation. An EGD was performed to assess the underlying etiology of anemia. Endoscopy revealed nodular erythematous lesions and erosions in the gastric antrum (See accompanying figures). Biopsies were taken at affected sites with normal appearing gross histological architecture of foveolar surface epithelium and underlying gastric crypts. However, Congo red staining of histological samples revealed amyloid deposition consistent with gastrointestinal amyloidosis. Following biopsy confirmed diagnosis of amyloid in the GI tract, a thorough workup for systemic amyloidosis was conducted (Table 1).
Discussion: Isolated gastric amyloidosis poses diagnostic challenges with only 28 cases reported in the literature. The gold standard for diagnosis of both forms is biopsy confirmation of amyloid deposition. The site of highest diagnostic yield for direct biopsy verification of disease is the duodenum followed by stomach, colon, rectum and esophagus. In the stomach, endoscopic findings can include gastric erosions, submucosal tumor-like masses, intramural hematomas, ulcerations, and rugal fold thickening. While the first-line therapy for localized AL amyloidosis is mainly supportive care, steroids, and the excision of amyloid deposits, for isolated gastric amyloidosis, endoscopic submucosal dissection (ESD) can be considered as a less invasive and potentially effective treatment for lesions confined to the stomach. Our case underscores the enigmatic nature of isolated gastric amyloidosis, emphasizing timely recognition through endoscopic evaluation and biopsy.

Figure: Fig.1 - Raised erythematous lesions in the gastric antrum
Fig.2 - Multiple friable lesions in the gastric antrum
Fig.3 - H&E gastric staining with normal foveolar surface epithelium and normal underlying gastric crypts
Fig.4 - Congo Red staining of gastric biopsy with characteristic green birefringence under polarized light reflecting amyloid deposition
Fig.2 - Multiple friable lesions in the gastric antrum
Fig.3 - H&E gastric staining with normal foveolar surface epithelium and normal underlying gastric crypts
Fig.4 - Congo Red staining of gastric biopsy with characteristic green birefringence under polarized light reflecting amyloid deposition
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Taras Halan indicated no relevant financial relationships.
Garrick Gu indicated no relevant financial relationships.
Taylor Seacor indicated no relevant financial relationships.
Mark Sterling indicated no relevant financial relationships.
David Jones indicated no relevant financial relationships.
Taras Halan, MD1, Garrick H. Gu, MD2, Taylor Seacor, MD2, Mark Sterling, MD1, David Jones, MD3. P3376 - An Unusual Case of Isolated Gastric Amyloidosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
