Monday Poster Session
Category: Stomach
P3378 - Equity, Heredity and Cancer Risk: Delayed Diagnosis of Gastric Cancer and Lynch Syndrome in an Uninsured Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shalva Eliava, MD
Englewood Hospital and Medical Center
Englewood, NJ
Presenting Author(s)
Award: Presidential Poster Award
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Areeba Nayyer, MD1, Dipal Patel, MD1
1Englewood Hospital and Medical Center, Englewood, NJ; 2Englewood Hospital and Medical Center, Bogota, NJ
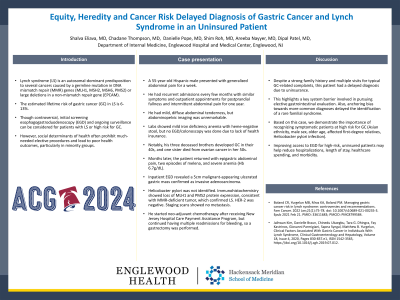
Introduction: Lynch syndrome (LS) is an autosomal-dominant predisposition to several cancers caused by a germline mutation in DNA mismatch repair (MMR) genes (MLH1, MSH2, MSH6, PMS2) or large deletions in a non-mismatch repair gene (EPCAM). The estimated lifetime risk of gastric cancer (GC) in LS is 6-13%. Though controversial, initial screening esophagogastroduodenoscopy (EGD) and ongoing surveillance can be considered for patients with LS or high risk for GC. However, social determinants of health often prohibit much-needed elective procedures and lead to poor health outcomes, particularly in minority groups.
Case Description/Methods: A 55-year-old Hispanic male presented with generalized abdominal pain for a week. He had recurrent admissions every few months with similar symptoms and outpatient appointments for postprandial fullness and intermittent abdominal pain for one year. He had mild, diffuse abdominal tenderness, but abdominopelvic imaging was unremarkable. Labs showed mild iron deficiency anemia with heme-negative stool, but no EGD/colonoscopy was done due to lack of health insurance. Notably, his three deceased brothers developed GC in their 40s, and one sister died from ovarian cancer in her 50s. Months later, the patient returned with epigastric abdominal pain, two episodes of melena, and severe anemia (Hb 6.7g/dL). Inpatient EGD revealed a 5cm malignant-appearing ulcerated gastric mass confirmed as invasive adenocarcinoma. Helicobacter pylori was not identified. Immunohistochemistry showed loss of MLH1 and PMS2 protein expression, consistent with MMR-deficient tumor, which confirmed LS. HER-2 was negative. Staging scans showed no metastasis. He started neo-adjuvant chemotherapy after receiving Charity Care but continued having multiple readmissions for bleeding, so a gastrectomy was performed.
Discussion: Despite a strong family history and multiple visits for typical GC-related complaints, this patient had a delayed diagnosis due to uninsurance. This highlights a key system barrier involved in pursuing elective gastrointestinal evaluation. Also, anchoring bias towards more common diagnoses delayed the identification of a rare familial syndrome. Based on this case, we demonstrate the importance of recognizing symptomatic patients at high risk for GC (Asian ethnicity, male sex, older age, affected first-degree relatives, Helicobacter pylori infection). Improving access to EGD for high-risk, uninsured patients may help reduce hospitalizations, length of stay, healthcare spending, and morbidity.
Disclosures:
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Areeba Nayyer, MD1, Dipal Patel, MD1. P3378 - Equity, Heredity and Cancer Risk: Delayed Diagnosis of Gastric Cancer and Lynch Syndrome in an Uninsured Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Areeba Nayyer, MD1, Dipal Patel, MD1
1Englewood Hospital and Medical Center, Englewood, NJ; 2Englewood Hospital and Medical Center, Bogota, NJ
Introduction: Lynch syndrome (LS) is an autosomal-dominant predisposition to several cancers caused by a germline mutation in DNA mismatch repair (MMR) genes (MLH1, MSH2, MSH6, PMS2) or large deletions in a non-mismatch repair gene (EPCAM). The estimated lifetime risk of gastric cancer (GC) in LS is 6-13%. Though controversial, initial screening esophagogastroduodenoscopy (EGD) and ongoing surveillance can be considered for patients with LS or high risk for GC. However, social determinants of health often prohibit much-needed elective procedures and lead to poor health outcomes, particularly in minority groups.
Case Description/Methods: A 55-year-old Hispanic male presented with generalized abdominal pain for a week. He had recurrent admissions every few months with similar symptoms and outpatient appointments for postprandial fullness and intermittent abdominal pain for one year. He had mild, diffuse abdominal tenderness, but abdominopelvic imaging was unremarkable. Labs showed mild iron deficiency anemia with heme-negative stool, but no EGD/colonoscopy was done due to lack of health insurance. Notably, his three deceased brothers developed GC in their 40s, and one sister died from ovarian cancer in her 50s. Months later, the patient returned with epigastric abdominal pain, two episodes of melena, and severe anemia (Hb 6.7g/dL). Inpatient EGD revealed a 5cm malignant-appearing ulcerated gastric mass confirmed as invasive adenocarcinoma. Helicobacter pylori was not identified. Immunohistochemistry showed loss of MLH1 and PMS2 protein expression, consistent with MMR-deficient tumor, which confirmed LS. HER-2 was negative. Staging scans showed no metastasis. He started neo-adjuvant chemotherapy after receiving Charity Care but continued having multiple readmissions for bleeding, so a gastrectomy was performed.
Discussion: Despite a strong family history and multiple visits for typical GC-related complaints, this patient had a delayed diagnosis due to uninsurance. This highlights a key system barrier involved in pursuing elective gastrointestinal evaluation. Also, anchoring bias towards more common diagnoses delayed the identification of a rare familial syndrome. Based on this case, we demonstrate the importance of recognizing symptomatic patients at high risk for GC (Asian ethnicity, male sex, older age, affected first-degree relatives, Helicobacter pylori infection). Improving access to EGD for high-risk, uninsured patients may help reduce hospitalizations, length of stay, healthcare spending, and morbidity.
Disclosures:
Shalva Eliava indicated no relevant financial relationships.
Chadane Thompson indicated no relevant financial relationships.
Danielle Pope indicated no relevant financial relationships.
Shim Roh indicated no relevant financial relationships.
Areeba Nayyer indicated no relevant financial relationships.
Dipal Patel indicated no relevant financial relationships.
Shalva Eliava, MD1, Chadane Thompson, MD1, Danielle Pope, MD2, Shim Roh, MD1, Areeba Nayyer, MD1, Dipal Patel, MD1. P3378 - Equity, Heredity and Cancer Risk: Delayed Diagnosis of Gastric Cancer and Lynch Syndrome in an Uninsured Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

