Monday Poster Session
Category: Stomach
P3385 - Collagenous Gastritis in a Young Adult: Diagnostic Challenges and Therapeutic Approaches
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rimmel Ali, MBBS
Dow Medical College, MA
Presenting Author(s)
Fariha Hasan, MD1, Rimmel Ali, MBBS2, Kim HooKim, MD3, Krysta Contino, MD4
1Cooper University Hospital, Philadelphia, PA; 2Dow Medical College, Karachi, Sindh, Pakistan; 3Cooper University Hospital, Camden, NJ; 4Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ
Introduction: Collagenous gastritis (CG) is a rare condition, often characterized by non-specific symptoms such as abdominal pain, nausea, vomiting, and diarrhea. Accurate diagnosis relies heavily on endoscopic examination and histological analyses, given its association with collagenous colitis and celiac disease. The limited number of reported cases underscores the need for a comprehensive understanding of CG for effective management and patient care.
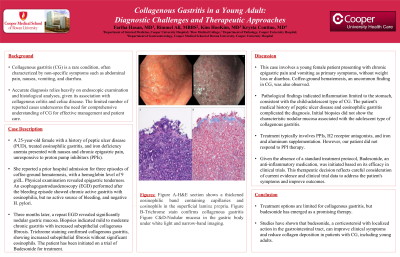
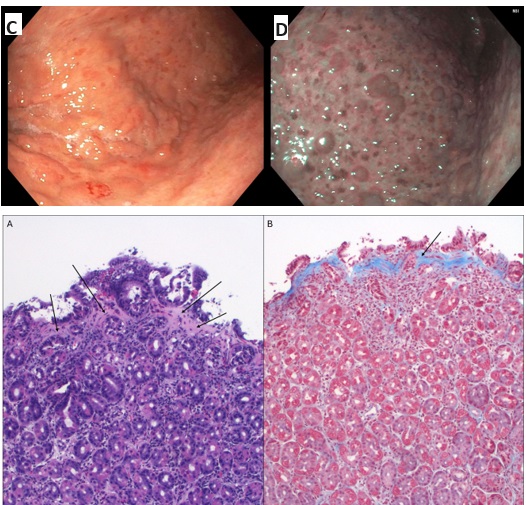
Case Description/Methods: A 25-year-old female with a history of peptic ulcer disease (PUD), treated eosinophilic gastritis, and iron deficiency anemia presented with nausea and chronic epigastric pain, unresponsive to proton pump inhibitors (PPIs). She reported a prior hospital admission for three episodes of coffee-ground emesis, with a hemoglobin level of 9 g/dL. Physical examination revealed epigastric tenderness. An esophagogastroduodenoscopy (EGD) performed after the bleeding episode showed chronic active gastritis with eosinophilia but no active source of bleeding and negative H. pylori. Three months later, a repeat EGD revealed significantly nodular gastric mucosa. Biopsies indicated mild to moderate chronic gastritis with increased subepithelial collagenous fibrosis. Trichrome staining confirmed collagenous gastritis, showing increased subepithelial fibrosis without significant eosinophils. The patient remains on twice daily proton pump inhibitor therapy with discussions about transition to budesonide therapy.
Discussion: This case involves a young female patient presenting with chronic epigastric pain and vomiting as primary symptoms, without weight loss or diarrhea. Coffee-ground emesis, an uncommon finding in CG, was also observed. Pathological findings indicated inflammation limited to the stomach, consistent with the child-adolescent type of CG. The patient's medical history of peptic ulcer disease and eosinophilic gastritis complicated the diagnosis.
Treatment typically involves PPIs, H2 receptor antagonists, and iron and aluminum supplementation. Budesonide has also been presented as a potential treatment, although given the lack of standard protocol, the risks and benefits of treatments must be discussed with patients and selected on a case-by-case basis. The therapeutic decision includes consideration of current evidence and clinical trial data to address the patient's symptoms and improve outcomes.
Disclosures:
Fariha Hasan, MD1, Rimmel Ali, MBBS2, Kim HooKim, MD3, Krysta Contino, MD4. P3385 - Collagenous Gastritis in a Young Adult: Diagnostic Challenges and Therapeutic Approaches, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Cooper University Hospital, Philadelphia, PA; 2Dow Medical College, Karachi, Sindh, Pakistan; 3Cooper University Hospital, Camden, NJ; 4Digestive Health Institute at Cooper University Hospital, Mount Laurel, NJ
Introduction: Collagenous gastritis (CG) is a rare condition, often characterized by non-specific symptoms such as abdominal pain, nausea, vomiting, and diarrhea. Accurate diagnosis relies heavily on endoscopic examination and histological analyses, given its association with collagenous colitis and celiac disease. The limited number of reported cases underscores the need for a comprehensive understanding of CG for effective management and patient care.
Case Description/Methods: A 25-year-old female with a history of peptic ulcer disease (PUD), treated eosinophilic gastritis, and iron deficiency anemia presented with nausea and chronic epigastric pain, unresponsive to proton pump inhibitors (PPIs). She reported a prior hospital admission for three episodes of coffee-ground emesis, with a hemoglobin level of 9 g/dL. Physical examination revealed epigastric tenderness. An esophagogastroduodenoscopy (EGD) performed after the bleeding episode showed chronic active gastritis with eosinophilia but no active source of bleeding and negative H. pylori. Three months later, a repeat EGD revealed significantly nodular gastric mucosa. Biopsies indicated mild to moderate chronic gastritis with increased subepithelial collagenous fibrosis. Trichrome staining confirmed collagenous gastritis, showing increased subepithelial fibrosis without significant eosinophils. The patient remains on twice daily proton pump inhibitor therapy with discussions about transition to budesonide therapy.
Discussion: This case involves a young female patient presenting with chronic epigastric pain and vomiting as primary symptoms, without weight loss or diarrhea. Coffee-ground emesis, an uncommon finding in CG, was also observed. Pathological findings indicated inflammation limited to the stomach, consistent with the child-adolescent type of CG. The patient's medical history of peptic ulcer disease and eosinophilic gastritis complicated the diagnosis.
Treatment typically involves PPIs, H2 receptor antagonists, and iron and aluminum supplementation. Budesonide has also been presented as a potential treatment, although given the lack of standard protocol, the risks and benefits of treatments must be discussed with patients and selected on a case-by-case basis. The therapeutic decision includes consideration of current evidence and clinical trial data to address the patient's symptoms and improve outcomes.
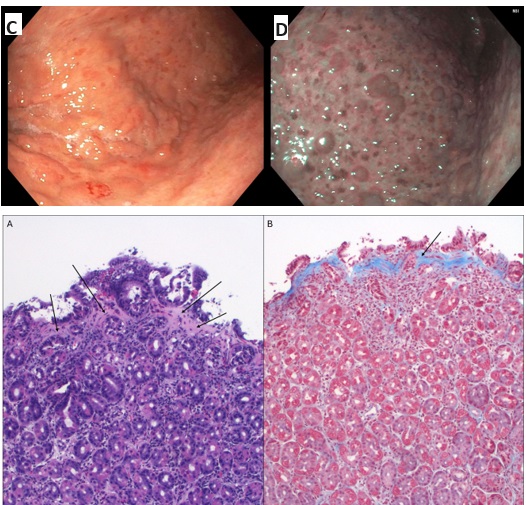
Figure: Figure A-H&E section shows a thickened eosinophilic band containing capillaries and eosinophils in the superficial lamina propria.
Figure B-Trichrome stain confirms collagenous gastritis
Figure C&D-Nodular mucosa in the gastric body under white light and narrow-band imaging
Figure B-Trichrome stain confirms collagenous gastritis
Figure C&D-Nodular mucosa in the gastric body under white light and narrow-band imaging
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Rimmel Ali indicated no relevant financial relationships.
Kim HooKim indicated no relevant financial relationships.
Krysta Contino indicated no relevant financial relationships.
Fariha Hasan, MD1, Rimmel Ali, MBBS2, Kim HooKim, MD3, Krysta Contino, MD4. P3385 - Collagenous Gastritis in a Young Adult: Diagnostic Challenges and Therapeutic Approaches, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
