Monday Poster Session
Category: Stomach
P3387 - A Rare Case of Collagenous Gastritis, Enteritis, and Colitis in an Elderly Female
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Parvir Aujla, MD
University of Texas Health, McGovern Medical School
Houston, TX
Presenting Author(s)
Parvir Aujla, MD1, Nitish Mittal, MD1, Abdullah S. Aleem, MD2, Christine Catinis, MD2, Maya C. Sarihan, MD2, Amreet Aujla, MD3
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas at Houston, Houston, TX; 3St. Agnes Medical Center, Fresno, CA
Introduction: The prevalence of collagenous gastritis is approximately 13 per 100,000. It is uncommon for patients to have collagenous gastritis with collagenous enteritis or colitis. We present a rare case of a 76-year-old female presenting with chronic diarrhea and unintentional weight loss, found to have a combination of collagenous gastritis, enteritis, and colitis.
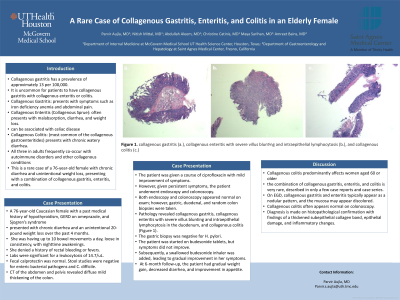
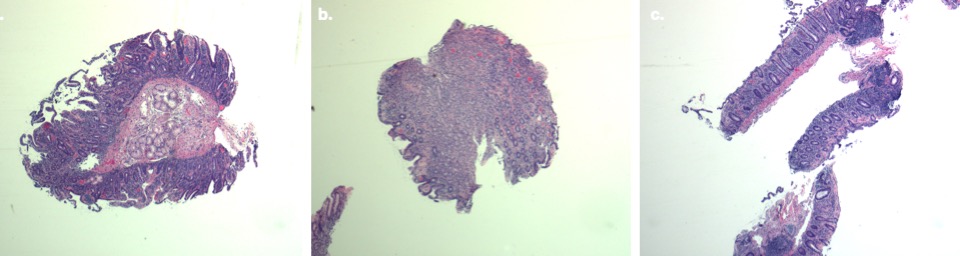
Case Description/Methods: A 76-year-old Caucasian female with a past medical history of hypothyroidism, GERD on omeprazole, and Sjogren’s syndrome presented with chronic diarrhea and an unintentional 20-pound weight loss over the past 4 months. She was having up to 10 bowel movements a day, loose in consistency, with nighttime awakenings. She denied a history of rectal bleeding or fevers. Labs were significant for a leukocytosis of 14.7/uL. Fecal calprotectin was normal. Stool studies were negative for enteric bacterial pathogens and C. difficile. A CT of the abdomen and pelvis revealed diffuse mild thickening of the colon. The patient was given a course of ciprofloxacin with mild improvement of symptoms. However, given persistent symptoms, the patient underwent endoscopy and colonoscopy. Both endoscopy and colonoscopy appeared normal on exam; however, gastric, duodenal, and random colon biopsies were taken. Pathology revealed collagenous gastritis, collagenous enteritis with severe villus blunting and intraepithelial lymphocytosis in the duodenum, and collagenous colitis (Figure 1). The gastric biopsy was negative for H. pylori. The patient was started on budesonide tablets, but symptoms did not improve. Subsequently, a swallowed budesonide inhaler was added, leading to gradual improvement in her symptoms. At 6-month follow-up, the patient had gradual weight gain, decreased diarrhea, and improvement in appetite.
Discussion: Collagenous colitis predominantly affects women aged 60 or older, and the combination of collagenous gastritis, enteritis, and colitis is very rare, described in only a few case reports and case series. On EGD, collagenous gastritis and enteritis typically appear as a nodular pattern, and the mucosa may appear discolored. Collagenous colitis often appears normal on colonoscopy. Diagnosis is made on histopathological confirmation with findings of a thickened subepithelial collagen band, epithelial damage, and inflammatory changes.
Disclosures:
Parvir Aujla, MD1, Nitish Mittal, MD1, Abdullah S. Aleem, MD2, Christine Catinis, MD2, Maya C. Sarihan, MD2, Amreet Aujla, MD3. P3387 - A Rare Case of Collagenous Gastritis, Enteritis, and Colitis in an Elderly Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Texas Health, McGovern Medical School, Houston, TX; 2University of Texas at Houston, Houston, TX; 3St. Agnes Medical Center, Fresno, CA
Introduction: The prevalence of collagenous gastritis is approximately 13 per 100,000. It is uncommon for patients to have collagenous gastritis with collagenous enteritis or colitis. We present a rare case of a 76-year-old female presenting with chronic diarrhea and unintentional weight loss, found to have a combination of collagenous gastritis, enteritis, and colitis.
Case Description/Methods: A 76-year-old Caucasian female with a past medical history of hypothyroidism, GERD on omeprazole, and Sjogren’s syndrome presented with chronic diarrhea and an unintentional 20-pound weight loss over the past 4 months. She was having up to 10 bowel movements a day, loose in consistency, with nighttime awakenings. She denied a history of rectal bleeding or fevers. Labs were significant for a leukocytosis of 14.7/uL. Fecal calprotectin was normal. Stool studies were negative for enteric bacterial pathogens and C. difficile. A CT of the abdomen and pelvis revealed diffuse mild thickening of the colon. The patient was given a course of ciprofloxacin with mild improvement of symptoms. However, given persistent symptoms, the patient underwent endoscopy and colonoscopy. Both endoscopy and colonoscopy appeared normal on exam; however, gastric, duodenal, and random colon biopsies were taken. Pathology revealed collagenous gastritis, collagenous enteritis with severe villus blunting and intraepithelial lymphocytosis in the duodenum, and collagenous colitis (Figure 1). The gastric biopsy was negative for H. pylori. The patient was started on budesonide tablets, but symptoms did not improve. Subsequently, a swallowed budesonide inhaler was added, leading to gradual improvement in her symptoms. At 6-month follow-up, the patient had gradual weight gain, decreased diarrhea, and improvement in appetite.
Discussion: Collagenous colitis predominantly affects women aged 60 or older, and the combination of collagenous gastritis, enteritis, and colitis is very rare, described in only a few case reports and case series. On EGD, collagenous gastritis and enteritis typically appear as a nodular pattern, and the mucosa may appear discolored. Collagenous colitis often appears normal on colonoscopy. Diagnosis is made on histopathological confirmation with findings of a thickened subepithelial collagen band, epithelial damage, and inflammatory changes.
Figure: Figure 1: collagenous gastritis (a.), collagenous enteritis with severe villus blunting and intraepithelial lymphocytosis (b.), and collagenous colitis (c.)
Disclosures:
Parvir Aujla indicated no relevant financial relationships.
Nitish Mittal indicated no relevant financial relationships.
Abdullah Aleem indicated no relevant financial relationships.
Christine Catinis indicated no relevant financial relationships.
Maya Sarihan indicated no relevant financial relationships.
Amreet Aujla indicated no relevant financial relationships.
Parvir Aujla, MD1, Nitish Mittal, MD1, Abdullah S. Aleem, MD2, Christine Catinis, MD2, Maya C. Sarihan, MD2, Amreet Aujla, MD3. P3387 - A Rare Case of Collagenous Gastritis, Enteritis, and Colitis in an Elderly Female, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
