Monday Poster Session
Category: Stomach
P3392 - Emphysematous Gastritis in a Patient With Choledocholithiasis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rafia Irfan Waheed, MBBS
University of South Dakota Sanford School of Medicine
Sioux Falls, SD
Presenting Author(s)
Rafia Irfan Waheed, MBBS1, Jyotroop Kaur, MBBS1, Gulzar Ahmed, MBBS2, Tony Oliver, MD1
1University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 2Dow University of Health Sciences, Sioux Falls, SD
Introduction: Emphysematous gastritis (EG) is a rare and life-threatening condition. It occurs when gas-forming microorganisms invade the gastric wall causing disruption in the gastric mucosa. Early diagnosis is crucial and can be aided by an urgent abdominal CT scan to identify characteristic gas within the stomach wall and associated vascular changes. Treatment involves immediate antibiotic therapy, intravenous fluid administration, and possible surgical intervention for severe cases. Hereby, we present a case of EG in a patient with non-obstructing choledocholithiasis.
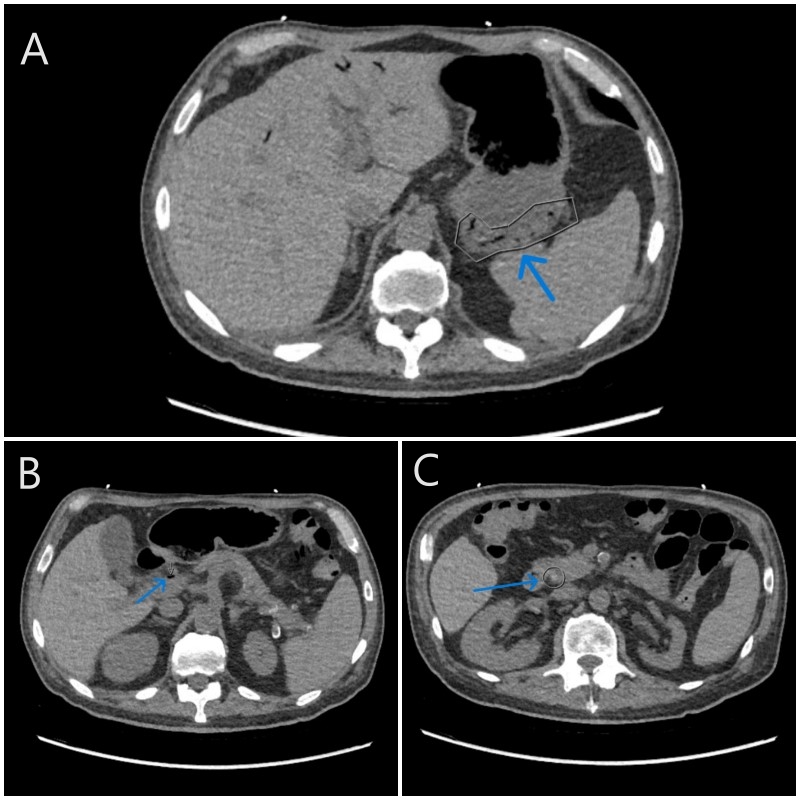
Case Description/Methods: A 65-year-old male with a medical history of, uncontrolled type 2 diabetes mellitus, chronic lymphocytic leukemia in remission, congestive heart failure, coronary artery disease, and non-obstructive choledocholithiasis presented to the emergency department with a high-grade fever, abdominal pain, nausea, and vomiting. He met the criteria for sepsis upon admission, and his blood work revealed an elevated white blood cell count and mildly abnormal liver function tests. A CT scan of his abdomen and pelvis showed signs of EG involving the fundus, along with gas around the perigastric region and in the portal venous system. The patient was hospitalized and promptly started on fluid resuscitation and piperacillin-tazobactam. His symptoms improved, and a follow-up CT scan five days later showed the resolution of emphysematous gastritis. He completed a 14-day antibiotic regimen. In this case, given EG occurred in the setting of choledocholithiasis the gastroenterology team recommended ERCP for removal of stones.
Discussion: Emphysematous gastritis is a severe and potentially fatal condition characterized by gastric necrosis and potential perforation if left untreated. Normally, the gastric wall is well-defended against bacterial invasion due to tight cellular connections, an acidic pH, and an adequate blood supply. However, factors like alcohol abuse, ingestion of corrosive substances, diabetes, and NSAID use can weaken these defenses, increasing the susceptibility to infection. In this case, we suspect the patient's underlying choledocholithiasis contributed to EG as it can lead to bile reflux, causing gastric mucosa erosion, bacterial imbalance, and elevated pH. Additionally, the patient's uncontrolled type 2 diabetes further increased their risk. This case underscores the significance of promptly addressing nonobstructing choledocholithiasis to prevent the development of EG.
Disclosures:
Rafia Irfan Waheed, MBBS1, Jyotroop Kaur, MBBS1, Gulzar Ahmed, MBBS2, Tony Oliver, MD1. P3392 - Emphysematous Gastritis in a Patient With Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of South Dakota Sanford School of Medicine, Sioux Falls, SD; 2Dow University of Health Sciences, Sioux Falls, SD
Introduction: Emphysematous gastritis (EG) is a rare and life-threatening condition. It occurs when gas-forming microorganisms invade the gastric wall causing disruption in the gastric mucosa. Early diagnosis is crucial and can be aided by an urgent abdominal CT scan to identify characteristic gas within the stomach wall and associated vascular changes. Treatment involves immediate antibiotic therapy, intravenous fluid administration, and possible surgical intervention for severe cases. Hereby, we present a case of EG in a patient with non-obstructing choledocholithiasis.
Case Description/Methods: A 65-year-old male with a medical history of, uncontrolled type 2 diabetes mellitus, chronic lymphocytic leukemia in remission, congestive heart failure, coronary artery disease, and non-obstructive choledocholithiasis presented to the emergency department with a high-grade fever, abdominal pain, nausea, and vomiting. He met the criteria for sepsis upon admission, and his blood work revealed an elevated white blood cell count and mildly abnormal liver function tests. A CT scan of his abdomen and pelvis showed signs of EG involving the fundus, along with gas around the perigastric region and in the portal venous system. The patient was hospitalized and promptly started on fluid resuscitation and piperacillin-tazobactam. His symptoms improved, and a follow-up CT scan five days later showed the resolution of emphysematous gastritis. He completed a 14-day antibiotic regimen. In this case, given EG occurred in the setting of choledocholithiasis the gastroenterology team recommended ERCP for removal of stones.
Discussion: Emphysematous gastritis is a severe and potentially fatal condition characterized by gastric necrosis and potential perforation if left untreated. Normally, the gastric wall is well-defended against bacterial invasion due to tight cellular connections, an acidic pH, and an adequate blood supply. However, factors like alcohol abuse, ingestion of corrosive substances, diabetes, and NSAID use can weaken these defenses, increasing the susceptibility to infection. In this case, we suspect the patient's underlying choledocholithiasis contributed to EG as it can lead to bile reflux, causing gastric mucosa erosion, bacterial imbalance, and elevated pH. Additionally, the patient's uncontrolled type 2 diabetes further increased their risk. This case underscores the significance of promptly addressing nonobstructing choledocholithiasis to prevent the development of EG.
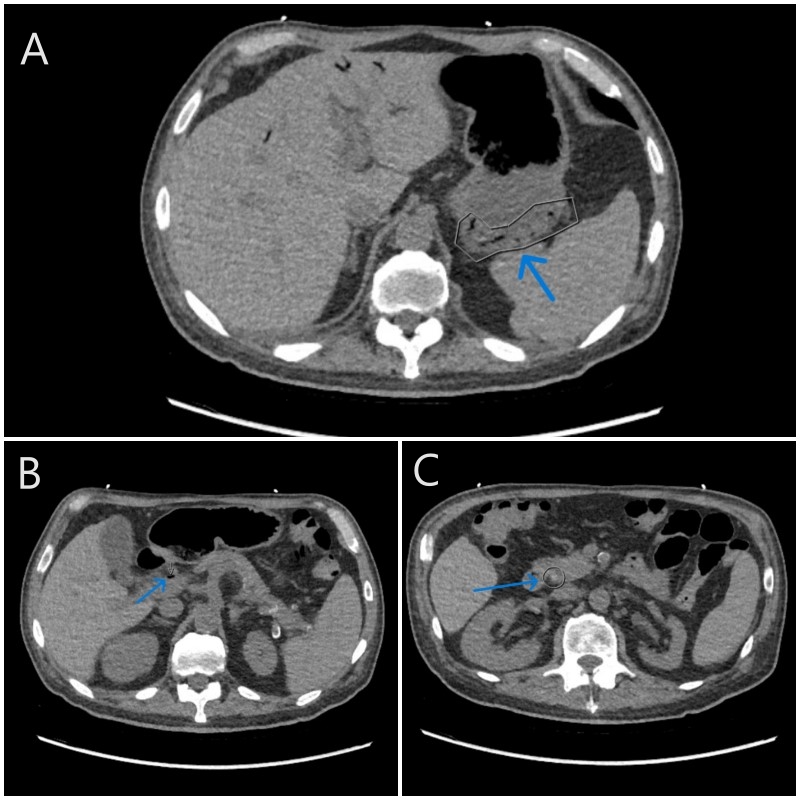
Figure: Figures A, B, and C: Blue arrows showing the features of Emphysematous Fundal Gastritis associated with perigastric and portal venous gas.
Disclosures:
Rafia Irfan Waheed indicated no relevant financial relationships.
Jyotroop Kaur indicated no relevant financial relationships.
Gulzar Ahmed indicated no relevant financial relationships.
Tony Oliver indicated no relevant financial relationships.
Rafia Irfan Waheed, MBBS1, Jyotroop Kaur, MBBS1, Gulzar Ahmed, MBBS2, Tony Oliver, MD1. P3392 - Emphysematous Gastritis in a Patient With Choledocholithiasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
