Monday Poster Session
Category: Stomach
P3410 - A Rare Case of an 11-cm Hamartomatous Gastric Polyp and Its Genetic Implications
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nader Al Souky, MD
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Nader Al Souky, MD1, Stephanie J. Melquist, MD1, Mahmoud Mahdi, MD1, Hasan Jaber, MD2, William J. Salyers, MD, MPH1
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas Medical Center, Wichita, KS
Introduction: Gastric polyps can manifest with gastrointestinal (GI) symptoms including dyspepsia, bloating, anemia and frank bleeding. Hamartomatous gastric polyps are extremely rare and occur in only one percent of cases. Their presence can pose challenges in endoscopic resection and should be identified due to their association of polyposis syndromes.
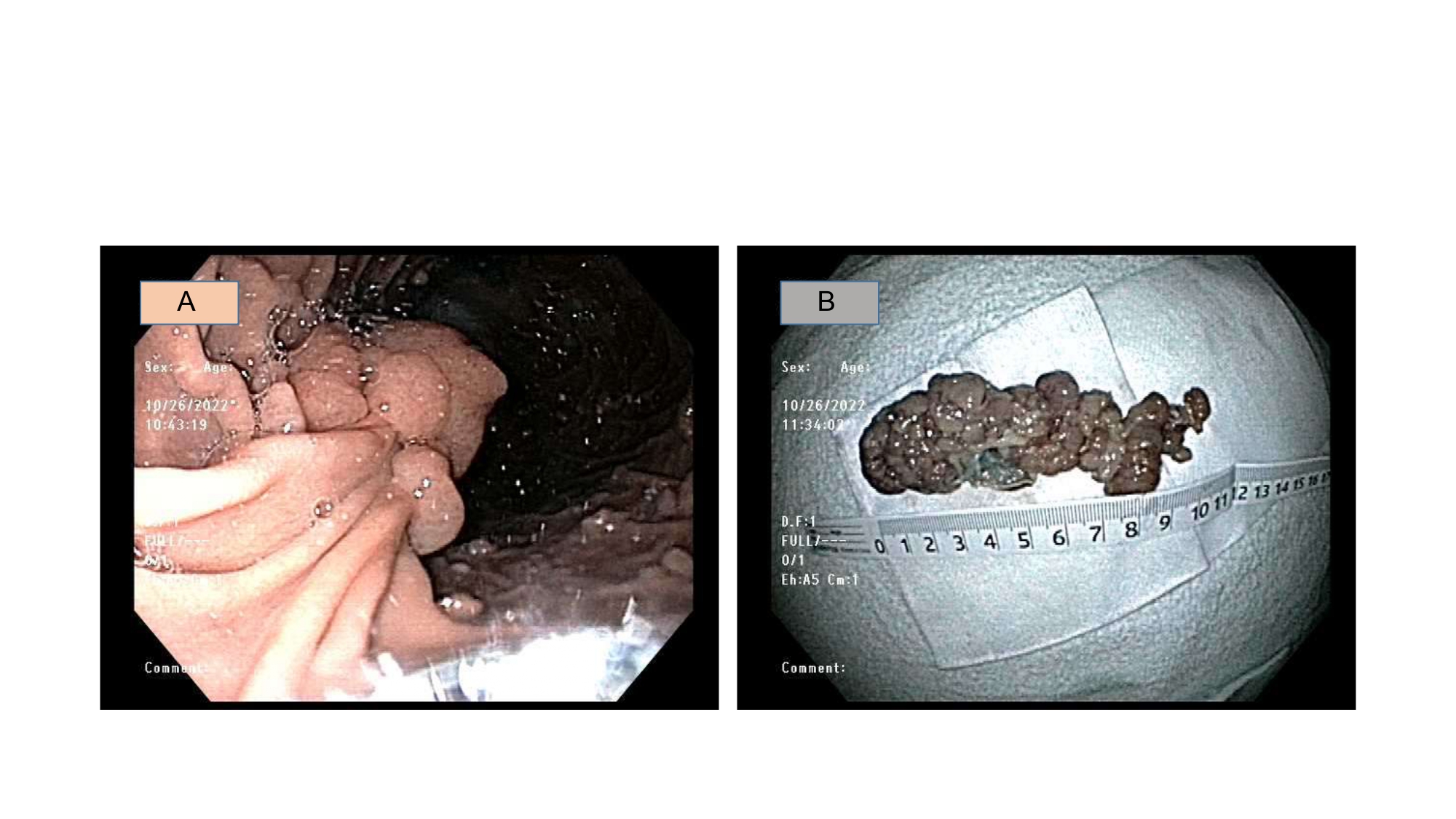
Case Description/Methods: A 49-year-old female with history of H. pylori gastritis, iron deficiency anemia despite supplementation and gastroesophageal reflux disease (GERD) presented to our ER for fatigue, dyspnea on exertion, melena, epigastric pain and hemoglobin (Hb) level of 4.6 g/dL. She had no history of NSAID or aspirin use, no alcohol or tobacco use, and no family history of GI malignancies. She was admitted to the hospital for stabilization and endoscopy. Urgent esophagogastroduodenoscopy (EGD) revealed a very large, pedunculated gastric polyp along the greater curvature measuring 11 cm following endoscopic mucosal piecemeal resection (Figure 1). Histology revealed cystically dilated, irregular glands with smooth muscle consistent with hamartomatous polyp. Following polyp resection, her anemia improved, and she had no further episodes of bleeding. Colonoscopy three months later revealed 3 advanced tubular adenomas. She was referred for genetic counseling to evaluate for potential polyposis syndromes which did not identify any genetic or hereditary syndromes.
Discussion: The incidence of symptomatic gastric polyps is low and are primarily of epithelial origin. Rarely, heterotopic polyps such as hamartomatous polyps, may be found. Hamartomatous polyps are seen in polyposis syndromes such as Peutz-Jeghers Syndrome, juvenile polyposis syndrome, or Cowden Syndrome. These syndromes may be sporadic or syndromic and are associated with increased risk of multiple malignancies. As such, patients with gastric hamartomatous polyps, particularly those larger than 1 cm, should undergo complete polyp resection for symptom alleviation and to ensure no underlying dysplasia or malignancy is found if present. Finally, these patients should be offered genetic counseling for polyposis syndromes to ensure that patients are offered all recommended cancer screening tests, even if they are without family history of these syndromes.
Disclosures:
Nader Al Souky, MD1, Stephanie J. Melquist, MD1, Mahmoud Mahdi, MD1, Hasan Jaber, MD2, William J. Salyers, MD, MPH1. P3410 - A Rare Case of an 11-cm Hamartomatous Gastric Polyp and Its Genetic Implications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas Medical Center, Wichita, KS
Introduction: Gastric polyps can manifest with gastrointestinal (GI) symptoms including dyspepsia, bloating, anemia and frank bleeding. Hamartomatous gastric polyps are extremely rare and occur in only one percent of cases. Their presence can pose challenges in endoscopic resection and should be identified due to their association of polyposis syndromes.
Case Description/Methods: A 49-year-old female with history of H. pylori gastritis, iron deficiency anemia despite supplementation and gastroesophageal reflux disease (GERD) presented to our ER for fatigue, dyspnea on exertion, melena, epigastric pain and hemoglobin (Hb) level of 4.6 g/dL. She had no history of NSAID or aspirin use, no alcohol or tobacco use, and no family history of GI malignancies. She was admitted to the hospital for stabilization and endoscopy. Urgent esophagogastroduodenoscopy (EGD) revealed a very large, pedunculated gastric polyp along the greater curvature measuring 11 cm following endoscopic mucosal piecemeal resection (Figure 1). Histology revealed cystically dilated, irregular glands with smooth muscle consistent with hamartomatous polyp. Following polyp resection, her anemia improved, and she had no further episodes of bleeding. Colonoscopy three months later revealed 3 advanced tubular adenomas. She was referred for genetic counseling to evaluate for potential polyposis syndromes which did not identify any genetic or hereditary syndromes.
Discussion: The incidence of symptomatic gastric polyps is low and are primarily of epithelial origin. Rarely, heterotopic polyps such as hamartomatous polyps, may be found. Hamartomatous polyps are seen in polyposis syndromes such as Peutz-Jeghers Syndrome, juvenile polyposis syndrome, or Cowden Syndrome. These syndromes may be sporadic or syndromic and are associated with increased risk of multiple malignancies. As such, patients with gastric hamartomatous polyps, particularly those larger than 1 cm, should undergo complete polyp resection for symptom alleviation and to ensure no underlying dysplasia or malignancy is found if present. Finally, these patients should be offered genetic counseling for polyposis syndromes to ensure that patients are offered all recommended cancer screening tests, even if they are without family history of these syndromes.
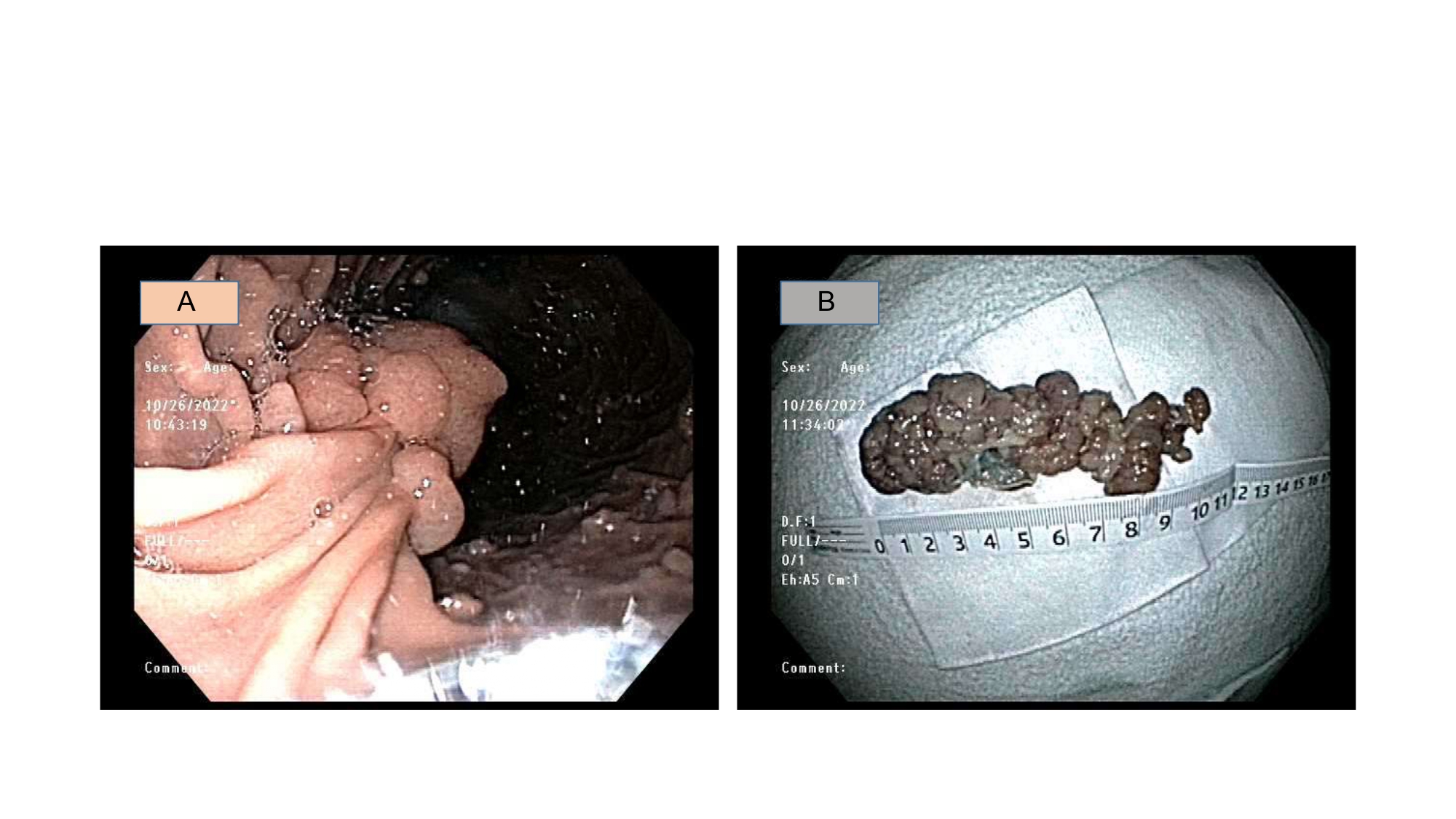
Figure: Figure 1: (A) Endoscopic View of Hamartomatous Gastric Polyp (B) Gross Examination of the 11-cm Polyp
Disclosures:
Nader Al Souky indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
Mahmoud Mahdi indicated no relevant financial relationships.
Hasan Jaber indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Nader Al Souky, MD1, Stephanie J. Melquist, MD1, Mahmoud Mahdi, MD1, Hasan Jaber, MD2, William J. Salyers, MD, MPH1. P3410 - A Rare Case of an 11-cm Hamartomatous Gastric Polyp and Its Genetic Implications, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
