Monday Poster Session
Category: Stomach
P3412 - Resolution of Gastric Ischemia Following Superior Mesenteric Artery Stenting in a Patient With Stage IV Pancreatic Adenocarcinoma
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Katherine Sorrentino, MD
Emory University School of Medicine
Atlanta, GA
Presenting Author(s)
Katherine Sorrentino, MD, Smit Deliwala, MD, Saurabh Chawla, MD
Emory University School of Medicine, Atlanta, GA
Introduction: The stomach has a robust vascular supply, primarily from the celiac and superior mesenteric arteries with their associated collaterals. As such, a lack of blood supply to the stomach to the degree of causing gastric ischemia is highly uncommon. When instances of localized or systemic vascular insufficiency lead to gastric ischemia, current practice focuses on supportive measures including volume resuscitation, antibiotics, and bowel rest. In severe cases not responding to these measures, surgical intervention may be warranted. Unfortunately, despite medical and surgical optimization, the overall prognosis for gastric ischemia is poor.
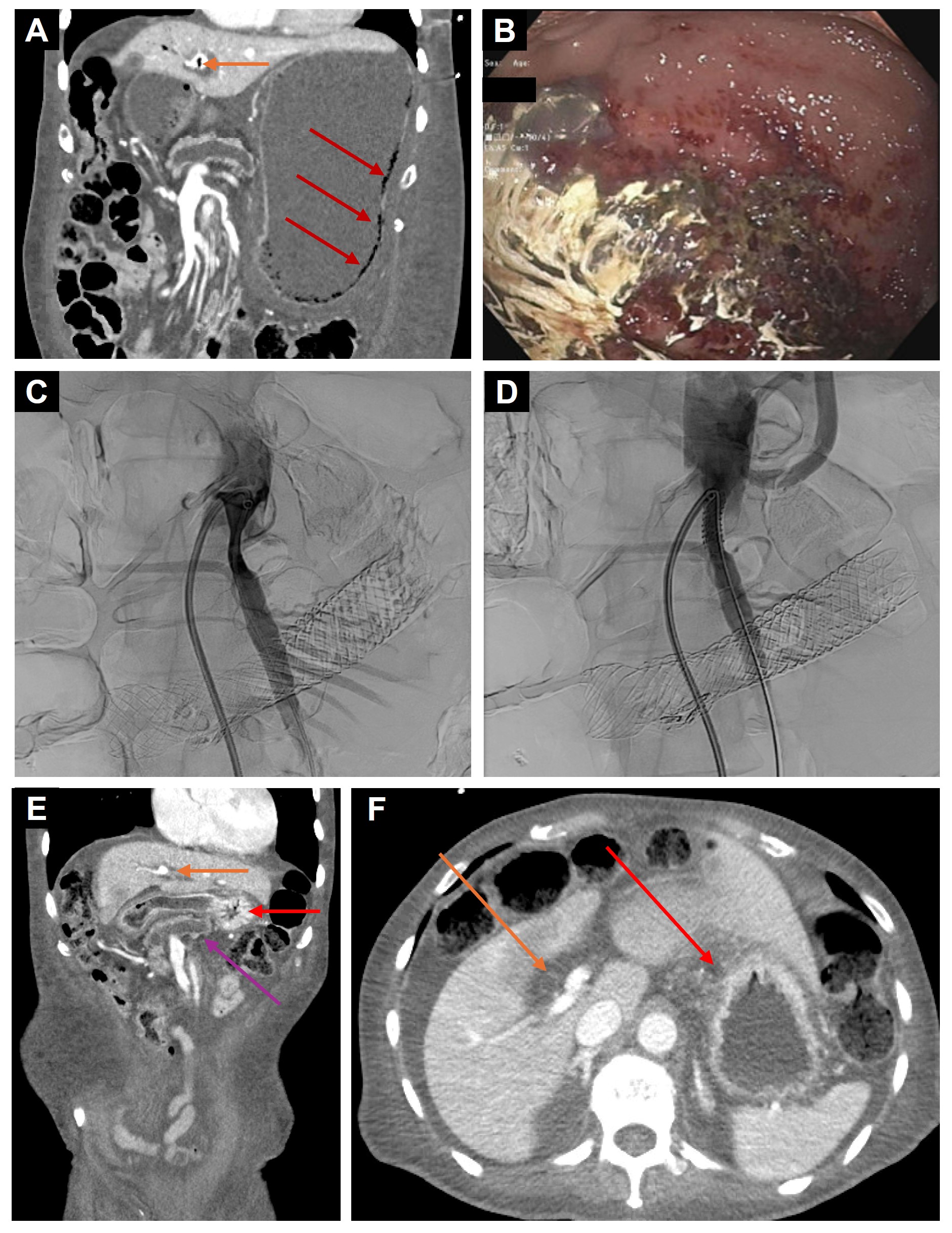
Case Description/Methods: A 62-year-old man with Stage IV Pancreatic Adenocarcinoma on chemotherapy, complicated by duodenal invasion with subsequent stent placement to the ascending duodenum, presented with emesis and epigastric pain. A CT scan of the abdomen showed signs of duodenal obstruction, as well as narrowing of the superior mesenteric artery (SMA) and celiac axis with new portal venous gas and gastric pneumatosis concerning for gastric ischemia. The patient underwent endoscopic stent-in-stent placement for the duodenal obstruction, and during the procedure was found to have evidence of ischemic gastritis involving the fundus of the stomach. In addition to medical management, the patient underwent endovascular stenting of the SMA with improved flow post-stent placement and interval resolution of pneumatosis and portal venous gas on subsequent CT scans. He had improvement in his symptoms and was ultimately able to tolerate oral intake and return home.
Discussion: In cases of gastric ischemia attributed to localized arterial stenosis from atherosclerotic disease, endovascular approaches have been successful in restoring blood supply to the stomach. This case demonstrates the utility of endovascular stenting in a patient with an extravascular etiology of vascular compromise. For patients with advanced pancreatic adenocarcinoma in which treatment options are limited, endovascular stenting to restore the gastric blood supply may prove valuable in the treatment of gastric ischemia and preserving quality of life.
Disclosures:
Katherine Sorrentino, MD, Smit Deliwala, MD, Saurabh Chawla, MD. P3412 - Resolution of Gastric Ischemia Following Superior Mesenteric Artery Stenting in a Patient With Stage IV Pancreatic Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Emory University School of Medicine, Atlanta, GA
Introduction: The stomach has a robust vascular supply, primarily from the celiac and superior mesenteric arteries with their associated collaterals. As such, a lack of blood supply to the stomach to the degree of causing gastric ischemia is highly uncommon. When instances of localized or systemic vascular insufficiency lead to gastric ischemia, current practice focuses on supportive measures including volume resuscitation, antibiotics, and bowel rest. In severe cases not responding to these measures, surgical intervention may be warranted. Unfortunately, despite medical and surgical optimization, the overall prognosis for gastric ischemia is poor.
Case Description/Methods: A 62-year-old man with Stage IV Pancreatic Adenocarcinoma on chemotherapy, complicated by duodenal invasion with subsequent stent placement to the ascending duodenum, presented with emesis and epigastric pain. A CT scan of the abdomen showed signs of duodenal obstruction, as well as narrowing of the superior mesenteric artery (SMA) and celiac axis with new portal venous gas and gastric pneumatosis concerning for gastric ischemia. The patient underwent endoscopic stent-in-stent placement for the duodenal obstruction, and during the procedure was found to have evidence of ischemic gastritis involving the fundus of the stomach. In addition to medical management, the patient underwent endovascular stenting of the SMA with improved flow post-stent placement and interval resolution of pneumatosis and portal venous gas on subsequent CT scans. He had improvement in his symptoms and was ultimately able to tolerate oral intake and return home.
Discussion: In cases of gastric ischemia attributed to localized arterial stenosis from atherosclerotic disease, endovascular approaches have been successful in restoring blood supply to the stomach. This case demonstrates the utility of endovascular stenting in a patient with an extravascular etiology of vascular compromise. For patients with advanced pancreatic adenocarcinoma in which treatment options are limited, endovascular stenting to restore the gastric blood supply may prove valuable in the treatment of gastric ischemia and preserving quality of life.
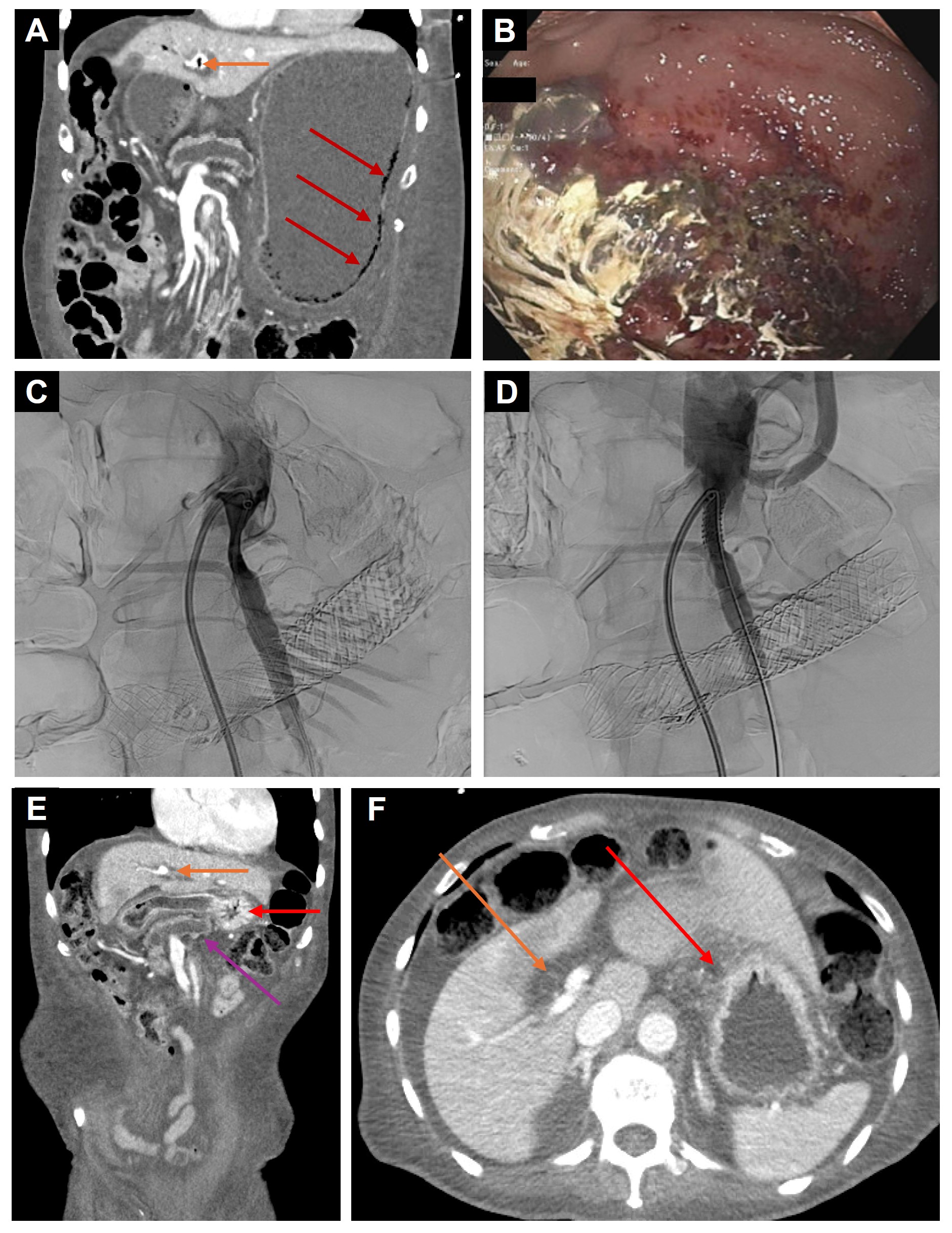
Figure: A. CT Abdomen and Pelvis coronal image demonstrating air depositing anti-dependently within the wall of the stomach consistent with gastric pneumatosis (red arrow) and gas within the intrahepatic main portal vein compatible with portal venous gas (orange arrow).
B. Mucosal changes seen in the gastric fundus on initial endoscopic evaluation.
C. Proximal superior mesenteric artery stenosis.
D. Superior mesenteric artery following stent placement.
E/F. Short-term 1-month follow-up CT abdomen and pelvis demonstrating resolution of gastric pneumatosis and portal venous gas (orange arrow = main portal vein, red arrow = stomach, purple arrow = dilated pancreatic duct).
B. Mucosal changes seen in the gastric fundus on initial endoscopic evaluation.
C. Proximal superior mesenteric artery stenosis.
D. Superior mesenteric artery following stent placement.
E/F. Short-term 1-month follow-up CT abdomen and pelvis demonstrating resolution of gastric pneumatosis and portal venous gas (orange arrow = main portal vein, red arrow = stomach, purple arrow = dilated pancreatic duct).
Disclosures:
Katherine Sorrentino indicated no relevant financial relationships.
Smit Deliwala indicated no relevant financial relationships.
Saurabh Chawla indicated no relevant financial relationships.
Katherine Sorrentino, MD, Smit Deliwala, MD, Saurabh Chawla, MD. P3412 - Resolution of Gastric Ischemia Following Superior Mesenteric Artery Stenting in a Patient With Stage IV Pancreatic Adenocarcinoma, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

