Tuesday Poster Session
Category: Biliary/Pancreas
P3449 - Unveiling the Hidden Impact: COVID-19's Influence on Acute Biliary Pancreatitis Outcomes in the United States
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Kibwey Peterkin, MD
One Brooklyn Health-Brookdale University Hospital Medical Center
Brooklyn, NY
Presenting Author(s)
Kibwey Peterkin, MD1, Shani Mc Lean, MD1, Carina-Leigh Lezama, MD2, Abiolah Telesford, MD1, Chidiebele Emmanuel Omaliko, MD1, Jamal Perry, MD1, Ifeanyi Uche, MD1
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Peterborough City Hospital, Peterborough, England, United Kingdom
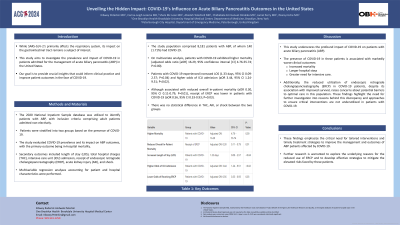
Introduction: While SARS-CoV-2's primary target is the respiratory system, its potential impact on the gastrointestinal tract remains a subject of intrigue. This study endeavors to investigate the impact of COVID-19 among patients admitted for acute biliary pancreatitis (ABP) in the United States. Join us as we delve into this unexplored territory, aiming to uncover crucial insights that could inform clinical practice and improve patient outcomes.
Methods: The 2020 National Inpatient Sample database was utilized to identify patients with ABP, with inclusion criteria comprising adult patients admitted non-electively. Patients were stratified into two groups based on the presence of COVID-19. The study evaluated COVID-19 prevalence and its impact on ABP outcomes, with the primary outcome being in-hospital mortality. Secondary outcomes included length of stay (LOS), total hospital charges (THC), intensive care unit (ICU) admission, endoscopic retrograde cholangiopancreatography (ERCP), acute kidney injury (AKI), and shock. Multivariable regression analyses, accounting for patient and hospital characteristics, were performed.
Results: The study population comprised 8,181 patients with ABP, of whom 140 (1.71%) had COVID-19. Patients with COVID-19 were more likely to be younger, Hispanic, and privately insured. Conversely, patients with COVID-19 were less likely to be male, or receive treatment in non-urban nonteaching hospitals. On multivariate analysis, patients with COVID-19 exhibited higher mortality (adjusted odds ratio [aOR] 16.29, 95% confidence interval [CI] 4.76-55.74; P=0.00). Additionally, patients with COVID-19 experienced increased LOS (1.33 days, 95% CI 0.09-2.57; P< 0.04) and higher odds of ICU admission (aOR 3.44, 95% CI 1.24-9.51; P< 0.02). Notably, although associated with reduced overall in-patient mortality (aOR 0.30, 95% CI 0.11-0.79; P=0.01), receipt of ERCP was lower in patients with COVID-19 (aOR 0.56, 95% CI 0.33-0.93; P=0.03). However, there was no statistical difference in THC, AKI, or shock between the two groups.
Discussion: COVID-19 is associated with higher mortality rates, longer hospital stays, and increased ICU admissions among ABP patients. Moreover, despite reduced overall mortality, COVID-19 patients are less likely to receive essential interventions such as ERCP. These findings underscore the need for tailored management strategies for ABP patients during the COVID-19 pandemic. Further research is needed to understand and address these disparities effectively.
Disclosures:
Kibwey Peterkin, MD1, Shani Mc Lean, MD1, Carina-Leigh Lezama, MD2, Abiolah Telesford, MD1, Chidiebele Emmanuel Omaliko, MD1, Jamal Perry, MD1, Ifeanyi Uche, MD1. P3449 - Unveiling the Hidden Impact: COVID-19's Influence on Acute Biliary Pancreatitis Outcomes in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 2Peterborough City Hospital, Peterborough, England, United Kingdom
Introduction: While SARS-CoV-2's primary target is the respiratory system, its potential impact on the gastrointestinal tract remains a subject of intrigue. This study endeavors to investigate the impact of COVID-19 among patients admitted for acute biliary pancreatitis (ABP) in the United States. Join us as we delve into this unexplored territory, aiming to uncover crucial insights that could inform clinical practice and improve patient outcomes.
Methods: The 2020 National Inpatient Sample database was utilized to identify patients with ABP, with inclusion criteria comprising adult patients admitted non-electively. Patients were stratified into two groups based on the presence of COVID-19. The study evaluated COVID-19 prevalence and its impact on ABP outcomes, with the primary outcome being in-hospital mortality. Secondary outcomes included length of stay (LOS), total hospital charges (THC), intensive care unit (ICU) admission, endoscopic retrograde cholangiopancreatography (ERCP), acute kidney injury (AKI), and shock. Multivariable regression analyses, accounting for patient and hospital characteristics, were performed.
Results: The study population comprised 8,181 patients with ABP, of whom 140 (1.71%) had COVID-19. Patients with COVID-19 were more likely to be younger, Hispanic, and privately insured. Conversely, patients with COVID-19 were less likely to be male, or receive treatment in non-urban nonteaching hospitals. On multivariate analysis, patients with COVID-19 exhibited higher mortality (adjusted odds ratio [aOR] 16.29, 95% confidence interval [CI] 4.76-55.74; P=0.00). Additionally, patients with COVID-19 experienced increased LOS (1.33 days, 95% CI 0.09-2.57; P< 0.04) and higher odds of ICU admission (aOR 3.44, 95% CI 1.24-9.51; P< 0.02). Notably, although associated with reduced overall in-patient mortality (aOR 0.30, 95% CI 0.11-0.79; P=0.01), receipt of ERCP was lower in patients with COVID-19 (aOR 0.56, 95% CI 0.33-0.93; P=0.03). However, there was no statistical difference in THC, AKI, or shock between the two groups.
Discussion: COVID-19 is associated with higher mortality rates, longer hospital stays, and increased ICU admissions among ABP patients. Moreover, despite reduced overall mortality, COVID-19 patients are less likely to receive essential interventions such as ERCP. These findings underscore the need for tailored management strategies for ABP patients during the COVID-19 pandemic. Further research is needed to understand and address these disparities effectively.
Disclosures:
Kibwey Peterkin indicated no relevant financial relationships.
Shani Mc Lean indicated no relevant financial relationships.
Carina-Leigh Lezama indicated no relevant financial relationships.
Abiolah Telesford indicated no relevant financial relationships.
Chidiebele Emmanuel Omaliko indicated no relevant financial relationships.
Jamal Perry indicated no relevant financial relationships.
Ifeanyi Uche indicated no relevant financial relationships.
Kibwey Peterkin, MD1, Shani Mc Lean, MD1, Carina-Leigh Lezama, MD2, Abiolah Telesford, MD1, Chidiebele Emmanuel Omaliko, MD1, Jamal Perry, MD1, Ifeanyi Uche, MD1. P3449 - Unveiling the Hidden Impact: COVID-19's Influence on Acute Biliary Pancreatitis Outcomes in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

