Tuesday Poster Session
Category: Biliary/Pancreas
P3460 - Comparative Assessment of Outcomes: Abdominal Drain vs No Abdominal Drain After Distal Pancreatectomy - A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Muhammad Jahanzaib Khan, MD
Mather Hospital, Northwell Health
New York, NY
Presenting Author(s)
Aleena Ahmed, MBBS1, Muhammad Jahanzaib Khan, MD2, Maurish Fatima, MBBS1, Muhammad Hammad Khan, MBBS1, Muhammad Hashim Faisal, MBBS1, Ayesha Sehar, MBBS1, Hassan Aziz, MD3
1King Edward Medical University, Lahore, Punjab, Pakistan; 2Mather Hospital, Northwell Health, New York, NY; 3University of Iowa, Iowa, IA
Introduction: Distal pancreatectomy (DP) is a surgical procedure commonly employed for various pancreatic conditions, often associated with postoperative complications like post-operative pancreatic fistula (POPF). While routine abdominal drainage following DP has been standard practice, recent evidence suggests potential benefits of omitting this approach. This systematic review and meta-analysis aimed to compare outcomes between abdominal drain placement and no drain placement post-pancreatectomy.
Methods: A comprehensive search was conducted on PubMed, Cochrane, and Embase from inception up to 15th March 2024, yielding nine studies comprising 15,817 patients. Data were extracted from randomized and non-randomized studies reporting primary and secondary outcomes. The analysis was performed in Revman. Risk ratios and Mean Difference were calculated with 95% confidence intervals, and a p-value of < 0.05 was considered statistically significant.
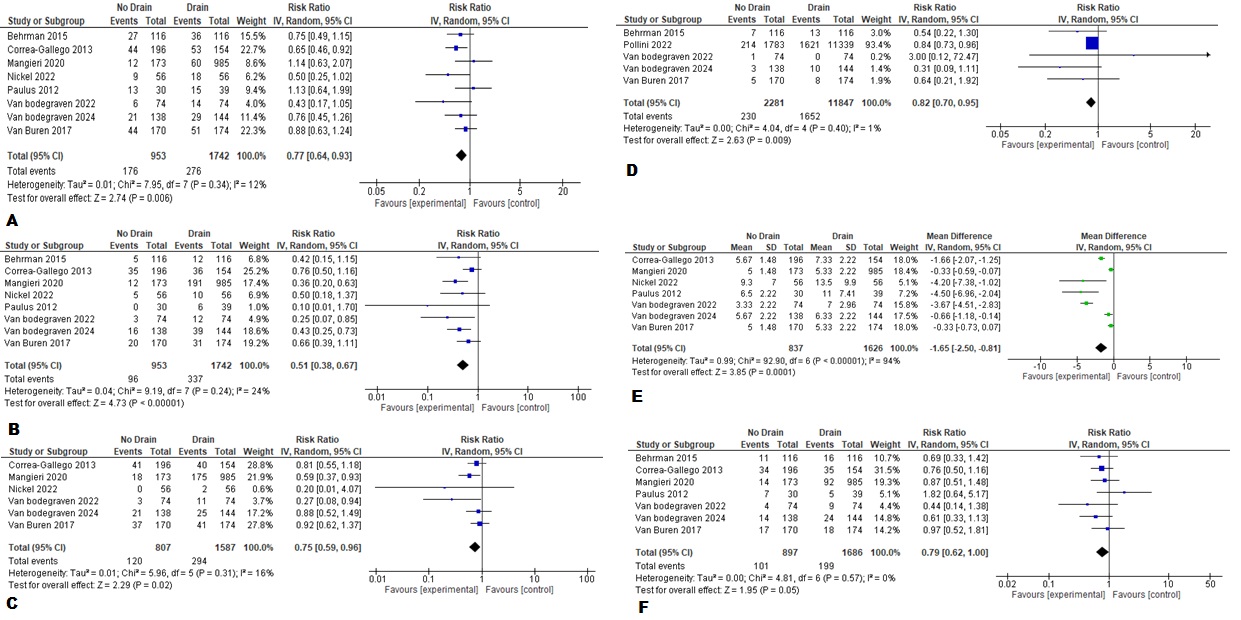
Results: A total of 13,081 patients underwent drain placement after distal pancreatectomy, and 2736 patients were included in the no-drain group. Out of the total, 45.1% (n= 7140) patients were male, with 45.9% (n= 6012) males in the drain group and 41.2% (n= 1128) males in the no-drain group. Major morbidity, defined as Clavien-Dindo grade ≥ III complications, was significantly lower in the no-drain group (RR: 0.77, 95% CI: 0.64 to 0.93, p = 0.006). Similarly, lower rates of POPF (RR: 0.51, 95% CI: 0.38 to 0.67, p < 0.00001), readmission (RR: 0.75, 95% CI: 0.59 to 0.96, p = 0.02), and surgical site infections (RR: 0.82, 95% CI: 0.70 to 0.95, p = 0.009) were observed in the no-drain group. Additionally, a shorter length of hospital stay was noted in this group (MD: -1.65, 95% CI: -2.50 to -0.81, p = 0.0001). There was no statistically significant association of post pancreatectomy hemorrhage, the need for radiological intervention, delayed gastric emptying, intra-abdominal abscess, re-operation, 30-day mortality, 90-day mortality, and Intensive Care Unit admission with any of the two groups.
Discussion: This study provides valuable insights into the debate surrounding postoperative drainage strategies in DP, suggesting the potential benefits of omitting routine abdominal drainage. However, further research is warranted to explore the impact of risk stratification, especially on various secondary outcomes, and validate our findings in diverse patient populations.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aleena Ahmed, MBBS1, Muhammad Jahanzaib Khan, MD2, Maurish Fatima, MBBS1, Muhammad Hammad Khan, MBBS1, Muhammad Hashim Faisal, MBBS1, Ayesha Sehar, MBBS1, Hassan Aziz, MD3. P3460 - Comparative Assessment of Outcomes: Abdominal Drain vs No Abdominal Drain After Distal Pancreatectomy - A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1King Edward Medical University, Lahore, Punjab, Pakistan; 2Mather Hospital, Northwell Health, New York, NY; 3University of Iowa, Iowa, IA
Introduction: Distal pancreatectomy (DP) is a surgical procedure commonly employed for various pancreatic conditions, often associated with postoperative complications like post-operative pancreatic fistula (POPF). While routine abdominal drainage following DP has been standard practice, recent evidence suggests potential benefits of omitting this approach. This systematic review and meta-analysis aimed to compare outcomes between abdominal drain placement and no drain placement post-pancreatectomy.
Methods: A comprehensive search was conducted on PubMed, Cochrane, and Embase from inception up to 15th March 2024, yielding nine studies comprising 15,817 patients. Data were extracted from randomized and non-randomized studies reporting primary and secondary outcomes. The analysis was performed in Revman. Risk ratios and Mean Difference were calculated with 95% confidence intervals, and a p-value of < 0.05 was considered statistically significant.
Results: A total of 13,081 patients underwent drain placement after distal pancreatectomy, and 2736 patients were included in the no-drain group. Out of the total, 45.1% (n= 7140) patients were male, with 45.9% (n= 6012) males in the drain group and 41.2% (n= 1128) males in the no-drain group. Major morbidity, defined as Clavien-Dindo grade ≥ III complications, was significantly lower in the no-drain group (RR: 0.77, 95% CI: 0.64 to 0.93, p = 0.006). Similarly, lower rates of POPF (RR: 0.51, 95% CI: 0.38 to 0.67, p < 0.00001), readmission (RR: 0.75, 95% CI: 0.59 to 0.96, p = 0.02), and surgical site infections (RR: 0.82, 95% CI: 0.70 to 0.95, p = 0.009) were observed in the no-drain group. Additionally, a shorter length of hospital stay was noted in this group (MD: -1.65, 95% CI: -2.50 to -0.81, p = 0.0001). There was no statistically significant association of post pancreatectomy hemorrhage, the need for radiological intervention, delayed gastric emptying, intra-abdominal abscess, re-operation, 30-day mortality, 90-day mortality, and Intensive Care Unit admission with any of the two groups.
Discussion: This study provides valuable insights into the debate surrounding postoperative drainage strategies in DP, suggesting the potential benefits of omitting routine abdominal drainage. However, further research is warranted to explore the impact of risk stratification, especially on various secondary outcomes, and validate our findings in diverse patient populations.
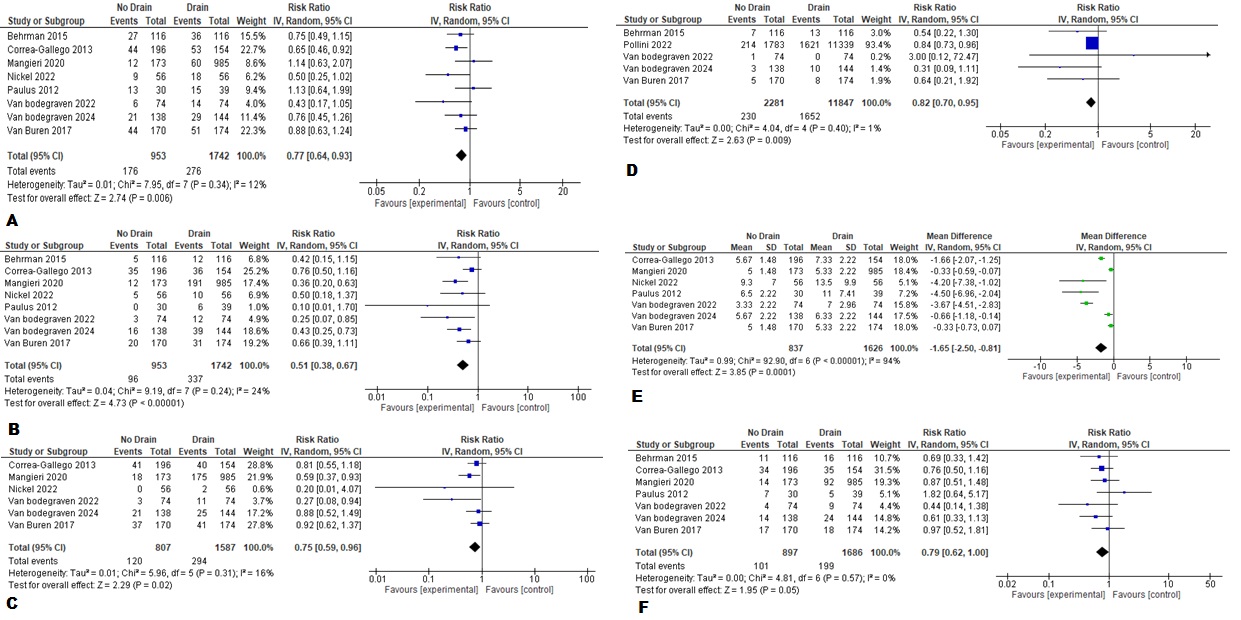
Figure: Figure (A) Forest plot Major morbidity (Clavien–Dindo grade ≥ III) (B) Forest Plot Postoperative pancreatic fistula, grade B/C (C) Forest Plot Readmission (D) Forest Plot Surgical Site Infections (E) Forest Plot Length of Hospital Stay (F) Forest Plot Radiological Intervention
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Aleena Ahmed indicated no relevant financial relationships.
Muhammad Jahanzaib Khan indicated no relevant financial relationships.
Maurish Fatima indicated no relevant financial relationships.
Muhammad Hammad Khan indicated no relevant financial relationships.
Muhammad Hashim Faisal indicated no relevant financial relationships.
Ayesha Sehar indicated no relevant financial relationships.
Hassan Aziz indicated no relevant financial relationships.
Aleena Ahmed, MBBS1, Muhammad Jahanzaib Khan, MD2, Maurish Fatima, MBBS1, Muhammad Hammad Khan, MBBS1, Muhammad Hashim Faisal, MBBS1, Ayesha Sehar, MBBS1, Hassan Aziz, MD3. P3460 - Comparative Assessment of Outcomes: Abdominal Drain vs No Abdominal Drain After Distal Pancreatectomy - A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
