Tuesday Poster Session
Category: Biliary/Pancreas
P3473 - Insights into Palliative Care Consultations for Pancreatic Cancer Admissions: A Six-Year Analysis of U.S. National Data
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Abhin Sapkota, MD
John H. Stroger, Jr. Hospital of Cook County
Chicago, IL
Presenting Author(s)
Abhin Sapkota, MD1, Alexandra Sueldo, MD1, Kriti Katwal, 2, Alejandro J. Nieto Dominguez, MD1, Daniel A. Guifarro, MD1, Bhanu Siva Mohan Pinnam, MD1
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Kathmandu, Bagmati, Nepal
Introduction: Pancreatic cancer (PC) patients have high mortality rates, with most cases diagnosed at an advanced stage. Despite advancements in treatment options, the overall prognosis remains poor. This emphasizes the importance of palliative care consultation (PCC) in such patients. This study aims to examine the rates of PCC among hospitalized PC patients from 2016 to 2021 and analyze the trend and underlying determinants.
Methods: A retrospective analysis of the National Inpatient Sample 2016 through 2021 was conducted to identify hospitalized patients with a primary diagnosis of PC using the International Classification of Diseases, 10th revision codes. Baseline hospitalization characteristics were highlighted and compared. A multivariate regression analysis was used to compare independent predictors of PCC. Trend analysis was done using logistic regression. A P-value of < 0.05 was considered statistically significant.
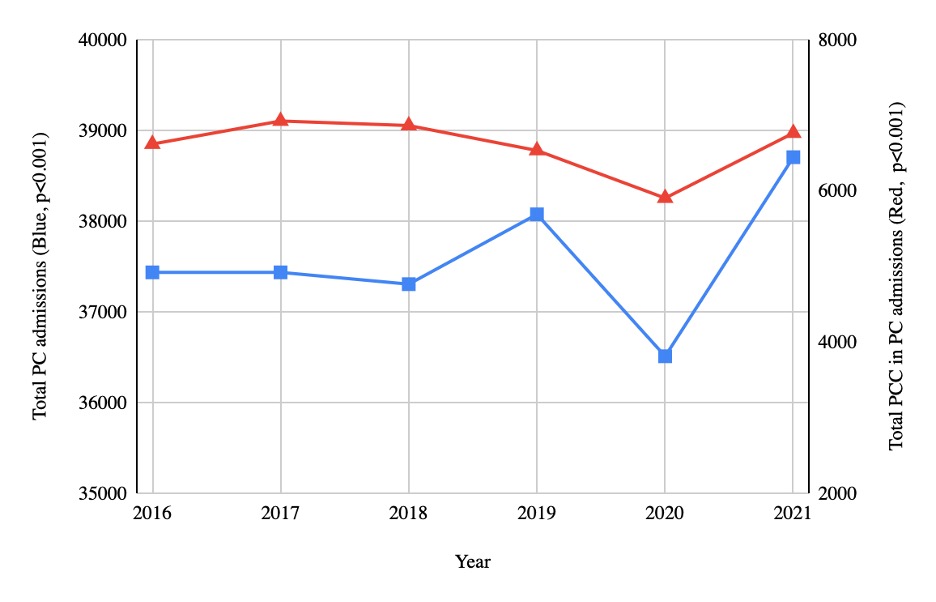
Results: Among the total 225, 665 admissions for PC, 39, 615 (17.6%) involved PCC. The mean age of those who received PCC was higher than that of total PC admissions (70.79 vs 68.32, p < 0.001). The mean cost was lower for admissions with PCC than total PC admissions (73672.09 vs 92064.46, p < 0.001). Blacks were more likely to receive PCC than whites (OR 1.27, p < 0.01). Amongst those patients who had Charlson comorbidity index (CCI) of 3 or more had higher odds of PCC compared to CCI of 2 (OR 2.56, p< 0.001). Medicaid patients had higher odds of PCC than Medicare (OR 1.43, p< 0.001). The longitudinal trend from 2016 to 2021 showed an increase in both total PC admissions and PCC.
Discussion:
Among PC patients, less than a quarter had PCC, indicating insufficient utilization of PCC. PC admissions have been increasing over the years, but PCCs are increasing at a lower rate than expected. Those with PCC had lower admission costs, indicating how PCC could potentially reduce healthcare costs. Those with multiple comorbidities had a higher rate of PCC, as these patients often have more complex health needs. Insurance also influences the likelihood of receiving a palliative care consult, which may reflect possible differences in healthcare delivery and policies. Blacks were more likely to receive PCC than whites, which is in contrast to the typical disparities among minorities. This may be likely due to differences in case presentation or cultural attitudes. These findings highlight critical areas of improvement needed for better delivery of palliative care to PC patients.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abhin Sapkota, MD1, Alexandra Sueldo, MD1, Kriti Katwal, 2, Alejandro J. Nieto Dominguez, MD1, Daniel A. Guifarro, MD1, Bhanu Siva Mohan Pinnam, MD1. P3473 - Insights into Palliative Care Consultations for Pancreatic Cancer Admissions: A Six-Year Analysis of U.S. National Data, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL; 2Lumbini Medical College, Kathmandu, Bagmati, Nepal
Introduction: Pancreatic cancer (PC) patients have high mortality rates, with most cases diagnosed at an advanced stage. Despite advancements in treatment options, the overall prognosis remains poor. This emphasizes the importance of palliative care consultation (PCC) in such patients. This study aims to examine the rates of PCC among hospitalized PC patients from 2016 to 2021 and analyze the trend and underlying determinants.
Methods: A retrospective analysis of the National Inpatient Sample 2016 through 2021 was conducted to identify hospitalized patients with a primary diagnosis of PC using the International Classification of Diseases, 10th revision codes. Baseline hospitalization characteristics were highlighted and compared. A multivariate regression analysis was used to compare independent predictors of PCC. Trend analysis was done using logistic regression. A P-value of < 0.05 was considered statistically significant.
Results: Among the total 225, 665 admissions for PC, 39, 615 (17.6%) involved PCC. The mean age of those who received PCC was higher than that of total PC admissions (70.79 vs 68.32, p < 0.001). The mean cost was lower for admissions with PCC than total PC admissions (73672.09 vs 92064.46, p < 0.001). Blacks were more likely to receive PCC than whites (OR 1.27, p < 0.01). Amongst those patients who had Charlson comorbidity index (CCI) of 3 or more had higher odds of PCC compared to CCI of 2 (OR 2.56, p< 0.001). Medicaid patients had higher odds of PCC than Medicare (OR 1.43, p< 0.001). The longitudinal trend from 2016 to 2021 showed an increase in both total PC admissions and PCC.
Discussion:
Among PC patients, less than a quarter had PCC, indicating insufficient utilization of PCC. PC admissions have been increasing over the years, but PCCs are increasing at a lower rate than expected. Those with PCC had lower admission costs, indicating how PCC could potentially reduce healthcare costs. Those with multiple comorbidities had a higher rate of PCC, as these patients often have more complex health needs. Insurance also influences the likelihood of receiving a palliative care consult, which may reflect possible differences in healthcare delivery and policies. Blacks were more likely to receive PCC than whites, which is in contrast to the typical disparities among minorities. This may be likely due to differences in case presentation or cultural attitudes. These findings highlight critical areas of improvement needed for better delivery of palliative care to PC patients.
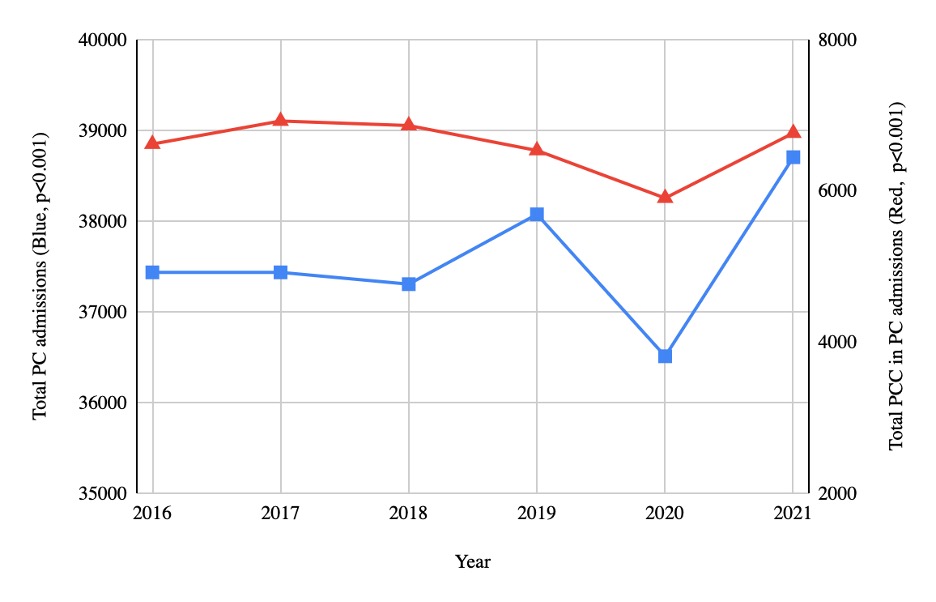
Figure: Trends in Palliative Care Consultations in Pancreatic Cancer Admissions
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Abhin Sapkota indicated no relevant financial relationships.
Alexandra Sueldo indicated no relevant financial relationships.
Kriti Katwal indicated no relevant financial relationships.
Alejandro Nieto Dominguez indicated no relevant financial relationships.
Daniel Guifarro indicated no relevant financial relationships.
Bhanu Siva Mohan Pinnam indicated no relevant financial relationships.
Abhin Sapkota, MD1, Alexandra Sueldo, MD1, Kriti Katwal, 2, Alejandro J. Nieto Dominguez, MD1, Daniel A. Guifarro, MD1, Bhanu Siva Mohan Pinnam, MD1. P3473 - Insights into Palliative Care Consultations for Pancreatic Cancer Admissions: A Six-Year Analysis of U.S. National Data, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
