Tuesday Poster Session
Category: Biliary/Pancreas
P3474 - Endoscopic Balloon Dilation vs Endoscopic Stent Placement in the Management of Dominant Strictures in Primary Sclerosing Cholangitis: A Systematic Review and Meta-Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Archit Garg, MD
Saint Peter's University Hospital
New Brunswick, NJ
Presenting Author(s)
Archit Garg, MD1, Vishali Moond, MD1, Tejas Nikumbh, MD2, Babu Mohan, MD3, Arkady Broder, MD1, Douglas Adler, MD4
1Saint Peter's University Hospital, New Brunswick, NJ; 2The Wright Center for Graduate Medical Education, Scanton, PA; 3Orlando Gastroenterology PA, Orlando, FL; 4Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
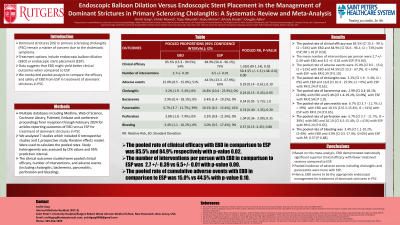
Introduction: Dominant strictures (DS) in primary sclerosing cholangitis (PSC) remain a matter of concern due to the cholestatic symptoms. Treatment options include endoscopic balloon dilation (EBD) or endoscopic stent placement (ESP). Data suggests that EBD might yield better clinical outcomes when compared to ESP. The objective of our study was to compare the efficacy and safety between the two.
Methods: We searched multiple databases including Medline, Web of Science, Cochrane Library, Pubmed, Embase and conference proceedings from inception through February 2024 for articles reporting outcomes of EBD versus ESP for treatment of dominant strictures in PSC. We studied the clinical efficacy, adverse events and transplantation rates among patients receiving these procedures. Standard meta-analysis methods were employed using the random-effects model, and heterogeneity was studied by I2 statistics.
Results: We analyzed 7 studies. There were 660 subjects, out of whom 244 subjects (mean age was 46.78 years) underwent EBD while 392 (mean age was 40.13 years) underwent ESP. 69% were males in the EBD group and 53.13% were males in ESP group. Number of interventions per person were 2.7 ± 0.39 with EBD and 6.5 ± 0.01 with ESP [SD 4.55 ± 1.3 (1.48 - 6.6); P 0.00]. Clinical efficacy was 85.5% [Cl 15.3 - 99.5; I2 = 54%] with EBD and 84.9% [Cl 56.6 - 96.1; I2 = 73%] with ESP; RR 1.01 [0.89 - 1.14; I2 = 72%; P 0.02]. Adverse events were higher with ESP, 44.5% [Cl 23.3 - 67.9%; I2 = 63%] compared to the EBD, 15.0% [Cl 8.5 - 15.0; I2 = 51%]; RR 0.29 [0.14 - 0.61; P 0.10]. Pancreatitis incidence was 6.7% [Cl 3.7 - 11.7%; I2 = 39%] and 10.1% [Cl 6.5-15.4%; I2 = 41%] with EBD and ESP respectively; RR 0.74 [0.40 - 1.35; P 0.20]. EBD caused less cholangitis, 3.2% [Cl 1.9 - 5.4%; I2 = 0%] compared to ESP, 16.8 [Cl 10.4 - 25.9%; I2 = 0%]; RR 0.24 [0.13 - 0.43; P 0.65]. Perforation rate was 3.8% [Cl 1.8 - 7.9%; I2 = 0%] and 3.3% [Cl 0.8 - 11.9%; I2 = 0%] with EBD and ESP respectively; RR 1.04 [0.36 - 2.99; I2 0.35]. Bleeding occurrence was 3.4% [Cl 1.1-10.2%; I2=0%] with EBD and 3.0% [Cl 0.5-17.4%; I2=0%] with ESP; RR 0.57 [0.13-2.45; P 0.88].
Discussion: Based on this meta-analysis, EBD demonstrated similar clinical efficacy with fewer treatment sessions. Moreover, incidence of adverse events including cholangitis and pancreatitis were more with ESP. Hence, EBD seems to be the appropriate endoscopic management for treatment of dominant strictures in PSC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Archit Garg, MD1, Vishali Moond, MD1, Tejas Nikumbh, MD2, Babu Mohan, MD3, Arkady Broder, MD1, Douglas Adler, MD4. P3474 - Endoscopic Balloon Dilation vs Endoscopic Stent Placement in the Management of Dominant Strictures in Primary Sclerosing Cholangitis: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Peter's University Hospital, New Brunswick, NJ; 2The Wright Center for Graduate Medical Education, Scanton, PA; 3Orlando Gastroenterology PA, Orlando, FL; 4Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: Dominant strictures (DS) in primary sclerosing cholangitis (PSC) remain a matter of concern due to the cholestatic symptoms. Treatment options include endoscopic balloon dilation (EBD) or endoscopic stent placement (ESP). Data suggests that EBD might yield better clinical outcomes when compared to ESP. The objective of our study was to compare the efficacy and safety between the two.
Methods: We searched multiple databases including Medline, Web of Science, Cochrane Library, Pubmed, Embase and conference proceedings from inception through February 2024 for articles reporting outcomes of EBD versus ESP for treatment of dominant strictures in PSC. We studied the clinical efficacy, adverse events and transplantation rates among patients receiving these procedures. Standard meta-analysis methods were employed using the random-effects model, and heterogeneity was studied by I2 statistics.
Results: We analyzed 7 studies. There were 660 subjects, out of whom 244 subjects (mean age was 46.78 years) underwent EBD while 392 (mean age was 40.13 years) underwent ESP. 69% were males in the EBD group and 53.13% were males in ESP group. Number of interventions per person were 2.7 ± 0.39 with EBD and 6.5 ± 0.01 with ESP [SD 4.55 ± 1.3 (1.48 - 6.6); P 0.00]. Clinical efficacy was 85.5% [Cl 15.3 - 99.5; I2 = 54%] with EBD and 84.9% [Cl 56.6 - 96.1; I2 = 73%] with ESP; RR 1.01 [0.89 - 1.14; I2 = 72%; P 0.02]. Adverse events were higher with ESP, 44.5% [Cl 23.3 - 67.9%; I2 = 63%] compared to the EBD, 15.0% [Cl 8.5 - 15.0; I2 = 51%]; RR 0.29 [0.14 - 0.61; P 0.10]. Pancreatitis incidence was 6.7% [Cl 3.7 - 11.7%; I2 = 39%] and 10.1% [Cl 6.5-15.4%; I2 = 41%] with EBD and ESP respectively; RR 0.74 [0.40 - 1.35; P 0.20]. EBD caused less cholangitis, 3.2% [Cl 1.9 - 5.4%; I2 = 0%] compared to ESP, 16.8 [Cl 10.4 - 25.9%; I2 = 0%]; RR 0.24 [0.13 - 0.43; P 0.65]. Perforation rate was 3.8% [Cl 1.8 - 7.9%; I2 = 0%] and 3.3% [Cl 0.8 - 11.9%; I2 = 0%] with EBD and ESP respectively; RR 1.04 [0.36 - 2.99; I2 0.35]. Bleeding occurrence was 3.4% [Cl 1.1-10.2%; I2=0%] with EBD and 3.0% [Cl 0.5-17.4%; I2=0%] with ESP; RR 0.57 [0.13-2.45; P 0.88].
Discussion: Based on this meta-analysis, EBD demonstrated similar clinical efficacy with fewer treatment sessions. Moreover, incidence of adverse events including cholangitis and pancreatitis were more with ESP. Hence, EBD seems to be the appropriate endoscopic management for treatment of dominant strictures in PSC.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Archit Garg indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Tejas Nikumbh indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Douglas Adler: Boston Scientific and Micro Tech. – Consultant.
Archit Garg, MD1, Vishali Moond, MD1, Tejas Nikumbh, MD2, Babu Mohan, MD3, Arkady Broder, MD1, Douglas Adler, MD4. P3474 - Endoscopic Balloon Dilation vs Endoscopic Stent Placement in the Management of Dominant Strictures in Primary Sclerosing Cholangitis: A Systematic Review and Meta-Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
