Tuesday Poster Session
Category: Biliary/Pancreas
P3481 - Clinical Predictors of Bacteremic Cholangitis: Results From a National Inpatient Sample (2016-2020) Based Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ruchir Damjibhai Paladiya, MBBS
University of Connecticut Health Center
Hartford, CT
Presenting Author(s)
Ruchir Damjibhai. Paladiya, MBBS1, Vikash Kumar, MD2, Vishali Moond, MD3, Sheza Malik, MD4, Murali Dharan, MD, MRCP5
1University of Connecticut Health Center, Hartford, CT; 2Creighton University School of Medicine, Brooklyn, NY; 3Saint Peter's University Hospital, New Brunswick, NJ; 4Rochester General Hospital, Rochester, NY; 5University of Connecticut Health Center, Farmington, CT
Introduction: Acute Cholangitis (AC) is a complex clinical syndrome with varying degrees of severity, from mild disease responsive to medical management to severe disease requiring urgent biliary decompression. Although studies have shown decreasing mortality related to AC (from 50% to 10-30%) there are still several unanswered questions about the factors that may influence the clinical course and prognosis. This study explores various factors associated with bacteremia and mortality among patients with cholangitis.
Methods: National Inpatient Sample (NIS) 2016–2020 was used to identify adult patients (age >18 years) with acute cholangitis using ICD-10 codes. Patients were stratified into two groups based on prevalence of bacteremia. The outcomes studied were prevalence of various clinical co-morbidities and its impact on mortality amongst the study population. A multivariate logistic regression analysis was performed to calculate the adjusted odds ratio (aOR) for the outcomes of interest.
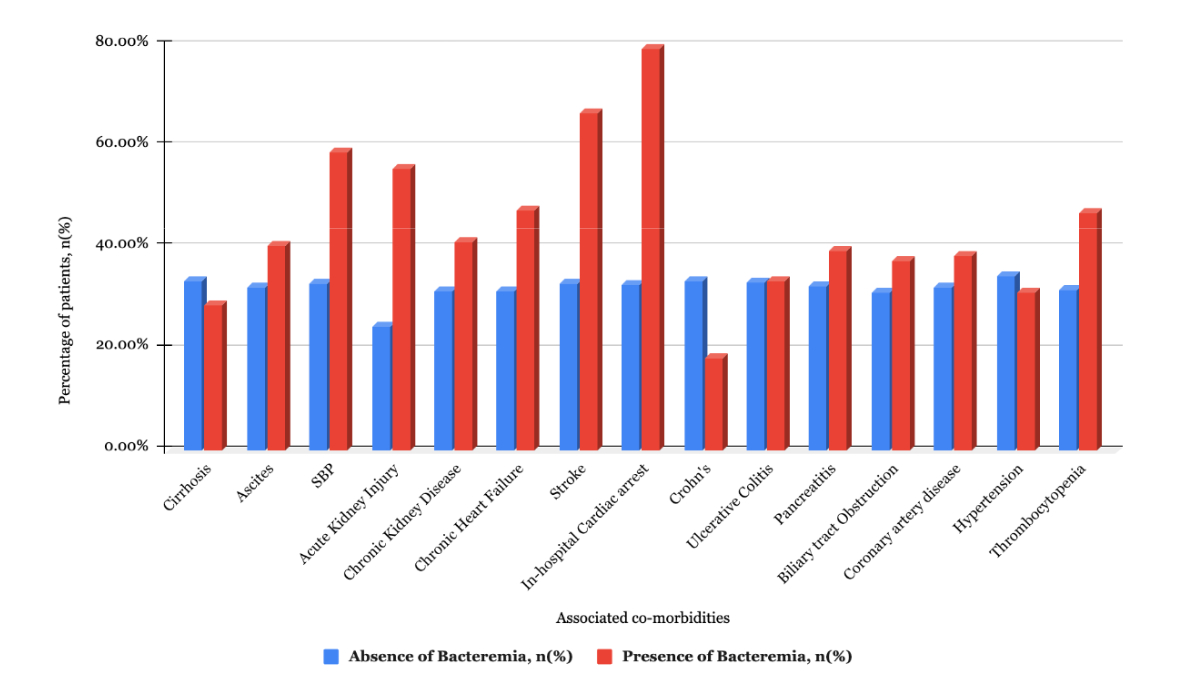
Results: Out of 43,860 patients with cholangitis, 14,540 patients (33.13%) had bacteremia. Figure 1 shows the prevalence of bacteremia among various co-morbidities. After adjusting for confounding factors, patients with bacteremia had higher prevalence of acute kidney injury (AKI) (aOR- 3.45, CI-3.28-3.63, p< 0.001), thrombocytopenia (TPN) (aOR- 1.66, CI-1.54-1.79, p< 0.001), chronic heart failure (CHF) (aOR- 1.34, CI-1.24-1.45, p< 0.001), ascites (aOR- 1.27, CI-1.18-1.37, p< 0.001), spontaneous bacterial peritonitis (aOR- 2.14, CI-1.66-2.75, p< 0.001), cerebrovascular accidents (CVA) (aOR- 3.18, CI-2.03-4.99, p< 0.001), pancreatitis (aOR- 1.21, CI-1.12-1.3, p< 0.001) and biliary tract obstruction (aOR- 1.32, CI-1.26-1.38, p< 0.001). (Table 1) After adjusting for confounding factors, factors associated with mortality were female sex, AKI, TPN, CHF, CVA, ascites, spontaneous bacterial peritonitis, bacteremia, septic shock and in-hospital cardiac arrest. (Table 1)
Discussion: Our analysis identified AKI, TPN, CHF, and CVA as independent risk factors for both bacteremia and mortality in the study population. Given the increased mortality observed in bacteremic cholangitis patients, further studies are warranted to explore the clinical and biochemical predictors of bacteremia. This also raises an important question of whether early endoscopic retrograde cholangiopancreatography amongst patients with higher odds of bacteremia could impact outcomes (morbidity and mortality).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ruchir Damjibhai. Paladiya, MBBS1, Vikash Kumar, MD2, Vishali Moond, MD3, Sheza Malik, MD4, Murali Dharan, MD, MRCP5. P3481 - Clinical Predictors of Bacteremic Cholangitis: Results From a National Inpatient Sample (2016-2020) Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut Health Center, Hartford, CT; 2Creighton University School of Medicine, Brooklyn, NY; 3Saint Peter's University Hospital, New Brunswick, NJ; 4Rochester General Hospital, Rochester, NY; 5University of Connecticut Health Center, Farmington, CT
Introduction: Acute Cholangitis (AC) is a complex clinical syndrome with varying degrees of severity, from mild disease responsive to medical management to severe disease requiring urgent biliary decompression. Although studies have shown decreasing mortality related to AC (from 50% to 10-30%) there are still several unanswered questions about the factors that may influence the clinical course and prognosis. This study explores various factors associated with bacteremia and mortality among patients with cholangitis.
Methods: National Inpatient Sample (NIS) 2016–2020 was used to identify adult patients (age >18 years) with acute cholangitis using ICD-10 codes. Patients were stratified into two groups based on prevalence of bacteremia. The outcomes studied were prevalence of various clinical co-morbidities and its impact on mortality amongst the study population. A multivariate logistic regression analysis was performed to calculate the adjusted odds ratio (aOR) for the outcomes of interest.
Results: Out of 43,860 patients with cholangitis, 14,540 patients (33.13%) had bacteremia. Figure 1 shows the prevalence of bacteremia among various co-morbidities. After adjusting for confounding factors, patients with bacteremia had higher prevalence of acute kidney injury (AKI) (aOR- 3.45, CI-3.28-3.63, p< 0.001), thrombocytopenia (TPN) (aOR- 1.66, CI-1.54-1.79, p< 0.001), chronic heart failure (CHF) (aOR- 1.34, CI-1.24-1.45, p< 0.001), ascites (aOR- 1.27, CI-1.18-1.37, p< 0.001), spontaneous bacterial peritonitis (aOR- 2.14, CI-1.66-2.75, p< 0.001), cerebrovascular accidents (CVA) (aOR- 3.18, CI-2.03-4.99, p< 0.001), pancreatitis (aOR- 1.21, CI-1.12-1.3, p< 0.001) and biliary tract obstruction (aOR- 1.32, CI-1.26-1.38, p< 0.001). (Table 1) After adjusting for confounding factors, factors associated with mortality were female sex, AKI, TPN, CHF, CVA, ascites, spontaneous bacterial peritonitis, bacteremia, septic shock and in-hospital cardiac arrest. (Table 1)
Discussion: Our analysis identified AKI, TPN, CHF, and CVA as independent risk factors for both bacteremia and mortality in the study population. Given the increased mortality observed in bacteremic cholangitis patients, further studies are warranted to explore the clinical and biochemical predictors of bacteremia. This also raises an important question of whether early endoscopic retrograde cholangiopancreatography amongst patients with higher odds of bacteremia could impact outcomes (morbidity and mortality).
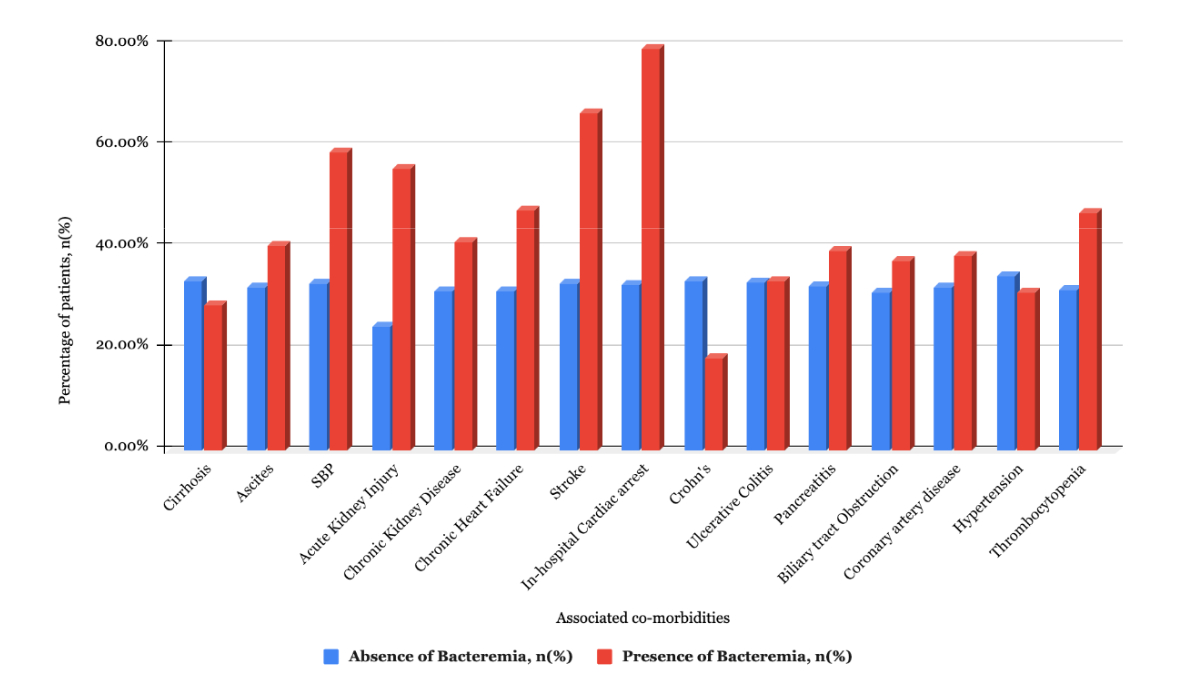
Figure: Figure 1. Prevalence of various co-morbidities in cholangitis patients, stratified by bacteremia.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ruchir Paladiya indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Sheza Malik indicated no relevant financial relationships.
Murali Dharan indicated no relevant financial relationships.
Ruchir Damjibhai. Paladiya, MBBS1, Vikash Kumar, MD2, Vishali Moond, MD3, Sheza Malik, MD4, Murali Dharan, MD, MRCP5. P3481 - Clinical Predictors of Bacteremic Cholangitis: Results From a National Inpatient Sample (2016-2020) Based Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

