Tuesday Poster Session
Category: Biliary/Pancreas
P3484 - Main Pancreatic Duct Sizing Discrepancies: Clinical Implications of EUS vs CT/MRI Findings
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Ramez M. Ibrahim, MD
University of Texas MD Anderson Cancer Center
Houston, TX
Presenting Author(s)
Ramez M.. Ibrahim, MD, Matt Manuel, PhD, Wei Qiao, PhD, Suresh T.. Chari, MD, Matthew H. G.. Katz, MD, Michael P.. Kim, MD, Manoop S.. Bhutani, MD, FACG
University of Texas MD Anderson Cancer Center, Houston, TX
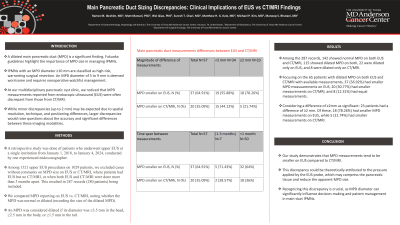
Introduction: A dilated main pancreatic duct (MPD) is a significant finding. Fukuoka guidelines highlight the importance of MPD size in managing intraductal papillary mucinous neoplasms (IPMNs). IPMNs with an MPD diameter ≥10 mm are classified as high-risk, warranting surgical resection. An MPD diameter of 5 to 9 mm is deemed worrisome and requires nonoperative watchful management. At our multidisciplinary pancreatic cyst clinic, we noticed that MPD measurements reported from endoscopic ultrasound (EUS) were often discrepant from those from CT/MRI. While minor discrepancies (up to 2 mm) may be expected due to spatial resolution, technique, and positioning differences, larger discrepancies would raise questions about the accuracy and significant differences between these imaging modalities.
Methods: A retrospective study was done of patients who underwent upper EUS at a single institution from January 1, 2018, to January 4, 2024, conducted by one experienced endosonographer. Among 1321 upper EUS procedures on 1029 patients, we excluded cases without comments on MPD size on EUS or CT/MRI, where patients had EUS but no CT/MRI, or when both EUS and CT/MRI were done more than 3 months apart. This resulted in 287 records (280 patients) being included. We compared MPD reporting on EUS vs. CT/MRI, noting whether the MPD was normal or dilated(recording the size of the dilated MPD). An MPD was considered dilated if its diameter was ≥3.5 mm in the head, ≥2.5 mm in the body, or ≥1.5 mm in the tail.
Results: Among the 287 records, 142 showed normal MPD on both EUS and CT/MRI, 115 showed dilated MPD on both, 22 were dilated only on EUS, and 8 were dilated only on CT/MRI. Focusing on the 65 patients with dilated MPD on both EUS and CT/MRI with available measurements, 37 (56.92%) had smaller MPD measurements on EUS, 20 (30.77%) had smaller measurements on CT/MRI, and 8 (12.31%) had equal measurements. Considering a difference of ≥2mm as significant: 23 patients had a difference of ≥2 mm. Of these, 18 (78.26%) had smaller MPD measurements on EUS, while 5 (21.74%) had smaller measurements on CT/MRI.
Discussion: Our study demonstrates that MPD measurements tend to be smaller on EUS compared to CT/MRI. This discrepancy could be theoretically attributed to the pressure applied by the EUS probe, which may compress the pancreatic tissue and reduce the apparent MPD size. Recognizing this discrepancy is crucial, as MPD diameter can significantly influence decision-making and patient management in main-duct IPMNs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramez M.. Ibrahim, MD, Matt Manuel, PhD, Wei Qiao, PhD, Suresh T.. Chari, MD, Matthew H. G.. Katz, MD, Michael P.. Kim, MD, Manoop S.. Bhutani, MD, FACG. P3484 - Main Pancreatic Duct Sizing Discrepancies: Clinical Implications of EUS vs CT/MRI Findings, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Texas MD Anderson Cancer Center, Houston, TX
Introduction: A dilated main pancreatic duct (MPD) is a significant finding. Fukuoka guidelines highlight the importance of MPD size in managing intraductal papillary mucinous neoplasms (IPMNs). IPMNs with an MPD diameter ≥10 mm are classified as high-risk, warranting surgical resection. An MPD diameter of 5 to 9 mm is deemed worrisome and requires nonoperative watchful management. At our multidisciplinary pancreatic cyst clinic, we noticed that MPD measurements reported from endoscopic ultrasound (EUS) were often discrepant from those from CT/MRI. While minor discrepancies (up to 2 mm) may be expected due to spatial resolution, technique, and positioning differences, larger discrepancies would raise questions about the accuracy and significant differences between these imaging modalities.
Methods: A retrospective study was done of patients who underwent upper EUS at a single institution from January 1, 2018, to January 4, 2024, conducted by one experienced endosonographer. Among 1321 upper EUS procedures on 1029 patients, we excluded cases without comments on MPD size on EUS or CT/MRI, where patients had EUS but no CT/MRI, or when both EUS and CT/MRI were done more than 3 months apart. This resulted in 287 records (280 patients) being included. We compared MPD reporting on EUS vs. CT/MRI, noting whether the MPD was normal or dilated(recording the size of the dilated MPD). An MPD was considered dilated if its diameter was ≥3.5 mm in the head, ≥2.5 mm in the body, or ≥1.5 mm in the tail.
Results: Among the 287 records, 142 showed normal MPD on both EUS and CT/MRI, 115 showed dilated MPD on both, 22 were dilated only on EUS, and 8 were dilated only on CT/MRI. Focusing on the 65 patients with dilated MPD on both EUS and CT/MRI with available measurements, 37 (56.92%) had smaller MPD measurements on EUS, 20 (30.77%) had smaller measurements on CT/MRI, and 8 (12.31%) had equal measurements. Considering a difference of ≥2mm as significant: 23 patients had a difference of ≥2 mm. Of these, 18 (78.26%) had smaller MPD measurements on EUS, while 5 (21.74%) had smaller measurements on CT/MRI.
Discussion: Our study demonstrates that MPD measurements tend to be smaller on EUS compared to CT/MRI. This discrepancy could be theoretically attributed to the pressure applied by the EUS probe, which may compress the pancreatic tissue and reduce the apparent MPD size. Recognizing this discrepancy is crucial, as MPD diameter can significantly influence decision-making and patient management in main-duct IPMNs.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Ramez Ibrahim indicated no relevant financial relationships.
Matt Manuel indicated no relevant financial relationships.
Wei Qiao indicated no relevant financial relationships.
Suresh Chari indicated no relevant financial relationships.
Matthew Katz indicated no relevant financial relationships.
Michael Kim indicated no relevant financial relationships.
Manoop Bhutani indicated no relevant financial relationships.
Ramez M.. Ibrahim, MD, Matt Manuel, PhD, Wei Qiao, PhD, Suresh T.. Chari, MD, Matthew H. G.. Katz, MD, Michael P.. Kim, MD, Manoop S.. Bhutani, MD, FACG. P3484 - Main Pancreatic Duct Sizing Discrepancies: Clinical Implications of EUS vs CT/MRI Findings, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
