Tuesday Poster Session
Category: Biliary/Pancreas
P3493 - Real World Analysis of Opiate Utilization and Pain Control in Chronic Pancreatitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NS
Nathaniel Scarberry, MD
University of Cincinnati Medical Center
Cincinnati, OH
Presenting Author(s)
Nathaniel Scarberry, MD, Andrew Ofosu, MD, MPH
University of Cincinnati Medical Center, Cincinnati, OH
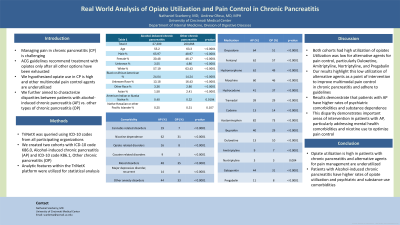
Introduction: Managing pain in chronic pancreatitis (CP) is challenging. ACG guidelines recommend treatment with opiates only after all other options have been exhausted. We hypothesize opiate use in CP is high and other multimodal pain control agents are underutilized. We further aimed to characterize disparities between patients with alcohol-induced chronic pancreatitis vs. other types of chronic pancreatitis.
Methods: TriNetX was queried using ICD-10 codes from all participating organizations. We created two cohorts with ICD-10 code K86.0, Alcohol-induced chronic pancreatitis (AP) and ICD-10 code K86.1, Other chronic pancreatitis (OP).
Results: We identified 220,868 patients in the OP cohort and 27,309 in the AP cohort. Patients with AP were younger than OP with a mean age of 55.2 vs. 63.3 (p-value < 0.0001) respectively. The AP cohort was predominantly male, 66% and white 57%. The OP cohort was 49% male and 64% white. Opiate use was higher in patients with AP vs. OP as follows: Oxycodone 64% vs. 51%, Fentanyl 62% vs. 57%, Hydromorphone 62% vs. 49%, Morphine 60% vs. 46%, Hydrocodone 41% vs. 37%, and Tramadol 39% vs. 29% (p value < 0.0001). Codeine was used more in OP 14% vs. 13% in AP (p value < 0.0001). Acetaminophen was prescribed in 82% in AP vs. 73% in OP (p value < 0.0001). Ibuprofen was prescribed in 40% of AP vs. 29% of OP (p value < 0.0001). Utilization of other medications was low in both cohorts. Duloxetine was prescribed in 13% in AP and 10% in OP (p value < 0.0001). Amitriptyline was prescribed in 9% of AP and 7% in OP (p value < 0.0001) and Nortriptyline in 3% of each cohort (p value 0.004). Gabapentin was prescribed in 44% of AP and 31% of OP and pregabalin in 11% of AP and 8% of OP (p value < 0.0001). Patients with AP compared to OP had higher rates of the following diagnoses: Cannabis related disorders 19% vs. 7%, Nicotine dependence 62% vs. 31%, opiate related disorders 16% vs. 8%, cocaine related disorders 9% vs. 3%, mood disorders 48% vs. 35%, major depressive disorder, recurrent 14% vs. 8%, and other anxiety disorders 44% vs. 33% (p values < 0.0001).
Discussion: Both cohorts had high utilization of opiates. Use of alternative agents for pain control was low. Our results highlight this as a point of intervention to improve multimodal pain control in CP and adhere to guidelines. Results demonstrate that patients with AP have higher rates of psychiatric comorbidities and substance use. This demonstrates important areas of intervention in patients with AP.
Disclosures:
Nathaniel Scarberry, MD, Andrew Ofosu, MD, MPH. P3493 - Real World Analysis of Opiate Utilization and Pain Control in Chronic Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Cincinnati Medical Center, Cincinnati, OH
Introduction: Managing pain in chronic pancreatitis (CP) is challenging. ACG guidelines recommend treatment with opiates only after all other options have been exhausted. We hypothesize opiate use in CP is high and other multimodal pain control agents are underutilized. We further aimed to characterize disparities between patients with alcohol-induced chronic pancreatitis vs. other types of chronic pancreatitis.
Methods: TriNetX was queried using ICD-10 codes from all participating organizations. We created two cohorts with ICD-10 code K86.0, Alcohol-induced chronic pancreatitis (AP) and ICD-10 code K86.1, Other chronic pancreatitis (OP).
Results: We identified 220,868 patients in the OP cohort and 27,309 in the AP cohort. Patients with AP were younger than OP with a mean age of 55.2 vs. 63.3 (p-value < 0.0001) respectively. The AP cohort was predominantly male, 66% and white 57%. The OP cohort was 49% male and 64% white. Opiate use was higher in patients with AP vs. OP as follows: Oxycodone 64% vs. 51%, Fentanyl 62% vs. 57%, Hydromorphone 62% vs. 49%, Morphine 60% vs. 46%, Hydrocodone 41% vs. 37%, and Tramadol 39% vs. 29% (p value < 0.0001). Codeine was used more in OP 14% vs. 13% in AP (p value < 0.0001). Acetaminophen was prescribed in 82% in AP vs. 73% in OP (p value < 0.0001). Ibuprofen was prescribed in 40% of AP vs. 29% of OP (p value < 0.0001). Utilization of other medications was low in both cohorts. Duloxetine was prescribed in 13% in AP and 10% in OP (p value < 0.0001). Amitriptyline was prescribed in 9% of AP and 7% in OP (p value < 0.0001) and Nortriptyline in 3% of each cohort (p value 0.004). Gabapentin was prescribed in 44% of AP and 31% of OP and pregabalin in 11% of AP and 8% of OP (p value < 0.0001). Patients with AP compared to OP had higher rates of the following diagnoses: Cannabis related disorders 19% vs. 7%, Nicotine dependence 62% vs. 31%, opiate related disorders 16% vs. 8%, cocaine related disorders 9% vs. 3%, mood disorders 48% vs. 35%, major depressive disorder, recurrent 14% vs. 8%, and other anxiety disorders 44% vs. 33% (p values < 0.0001).
Discussion: Both cohorts had high utilization of opiates. Use of alternative agents for pain control was low. Our results highlight this as a point of intervention to improve multimodal pain control in CP and adhere to guidelines. Results demonstrate that patients with AP have higher rates of psychiatric comorbidities and substance use. This demonstrates important areas of intervention in patients with AP.
Disclosures:
Nathaniel Scarberry indicated no relevant financial relationships.
Andrew Ofosu indicated no relevant financial relationships.
Nathaniel Scarberry, MD, Andrew Ofosu, MD, MPH. P3493 - Real World Analysis of Opiate Utilization and Pain Control in Chronic Pancreatitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

