Tuesday Poster Session
Category: Biliary/Pancreas
P3494 - GLP-1 RA Does Not Increase the Risk of Pancreatitis in Patients with Type 2 Diabetes Mellitus: A U.S. Based Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mark Ayoub, MD
West Virginia University - Charleston Area Medical Center
Charleston, WV
Presenting Author(s)
Mark Ayoub, MD1, Carol Faris, MD2, Harleen Chela, MD1, Veysel Tahan, MD1, Roberta Hunter, MD1, Ebubekir Daglilar, MD1
1West Virginia University - Charleston Area Medical Center, Charleston, WV; 2CarePoint Health - Bayonne Medical Center, Charleston, WV
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RA) are common medications for treating Type 2 Diabetes Mellitus (T2DM). The discussion surrounding the use GLP-1 RA in diabetes and the potential risk for pancreatitis is complex and multifaceted. While GLP-1 RA offer significant benefits in glycemic control and cardiovascular outcomes, concerns persist regarding their association with pancreatitis. Our study aims to highlight the association between GLP-1 RA use and the risk of pancreatitis.
Methods: We queried the US Collaborative Network (61 healthcare organizations) of TriNetX research database. Patients with T2DM were identified and divided into two cohorts; patients on GLP-1 RAs, and second cohort patients not on GLP-1 RAs. GLP-1 RAs included were: dulaglutide, lixisenatide, exenatide, liraglutide, and semaglutide. We compared the risk of pancreatitis over time between the two cohorts after using 1:1 propensity-scored matching (PSM) model using patients’ baseline demographics, comorbidities, medications-received, and lab values. Comorbidities used for PSM were hypertensive diseases, ischemic heart diseases, gallstones, annular pancreas, alcohol-use disorders, hypertriglyceridemia, hypercalcemia, cystic fibrosis, and cannabis use. Medications used in PSM are known to cause drug-induced pancreatitis. A full list of PSM components is highlighted in table 1.
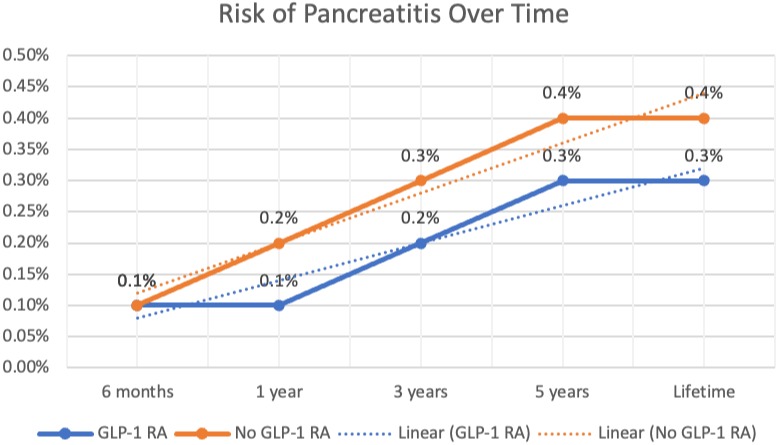
Results: 969,240 patients with T2DM were identified. Of those, 9.7% (93,608) were on GLP-1 RA, and 90.3% (875,632) were not. After propensity-score matching, the sample included 81,872 on GLP-1 RA and 81,872 not on GLP-1 RA. The risk of pancreatitis between the two groups were similar at 6 months at (0.1% vs 0.1%, p=0.04), the risk does not increase with time; at 1 year (0.1% vs 0.2%, p=0.02), 3 years (0.2% vs 0.3%, p=0.001), and 5 years (0.3% vs 0.4%, p< 0.001). The lifetime risk of developing pancreatitis in patients on GLP-1 RA was lower (0.3% vs 0.4%, p< 0.001).
Discussion: The use of GLP-1 RA in patients with T2DM does not increase their risk of pancreatitis. In fact, their use is associated with lower lifetime risk of pancreatitis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mark Ayoub, MD1, Carol Faris, MD2, Harleen Chela, MD1, Veysel Tahan, MD1, Roberta Hunter, MD1, Ebubekir Daglilar, MD1. P3494 - GLP-1 RA Does Not Increase the Risk of Pancreatitis in Patients with Type 2 Diabetes Mellitus: A U.S. Based Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1West Virginia University - Charleston Area Medical Center, Charleston, WV; 2CarePoint Health - Bayonne Medical Center, Charleston, WV
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1 RA) are common medications for treating Type 2 Diabetes Mellitus (T2DM). The discussion surrounding the use GLP-1 RA in diabetes and the potential risk for pancreatitis is complex and multifaceted. While GLP-1 RA offer significant benefits in glycemic control and cardiovascular outcomes, concerns persist regarding their association with pancreatitis. Our study aims to highlight the association between GLP-1 RA use and the risk of pancreatitis.
Methods: We queried the US Collaborative Network (61 healthcare organizations) of TriNetX research database. Patients with T2DM were identified and divided into two cohorts; patients on GLP-1 RAs, and second cohort patients not on GLP-1 RAs. GLP-1 RAs included were: dulaglutide, lixisenatide, exenatide, liraglutide, and semaglutide. We compared the risk of pancreatitis over time between the two cohorts after using 1:1 propensity-scored matching (PSM) model using patients’ baseline demographics, comorbidities, medications-received, and lab values. Comorbidities used for PSM were hypertensive diseases, ischemic heart diseases, gallstones, annular pancreas, alcohol-use disorders, hypertriglyceridemia, hypercalcemia, cystic fibrosis, and cannabis use. Medications used in PSM are known to cause drug-induced pancreatitis. A full list of PSM components is highlighted in table 1.
Results: 969,240 patients with T2DM were identified. Of those, 9.7% (93,608) were on GLP-1 RA, and 90.3% (875,632) were not. After propensity-score matching, the sample included 81,872 on GLP-1 RA and 81,872 not on GLP-1 RA. The risk of pancreatitis between the two groups were similar at 6 months at (0.1% vs 0.1%, p=0.04), the risk does not increase with time; at 1 year (0.1% vs 0.2%, p=0.02), 3 years (0.2% vs 0.3%, p=0.001), and 5 years (0.3% vs 0.4%, p< 0.001). The lifetime risk of developing pancreatitis in patients on GLP-1 RA was lower (0.3% vs 0.4%, p< 0.001).
Discussion: The use of GLP-1 RA in patients with T2DM does not increase their risk of pancreatitis. In fact, their use is associated with lower lifetime risk of pancreatitis.
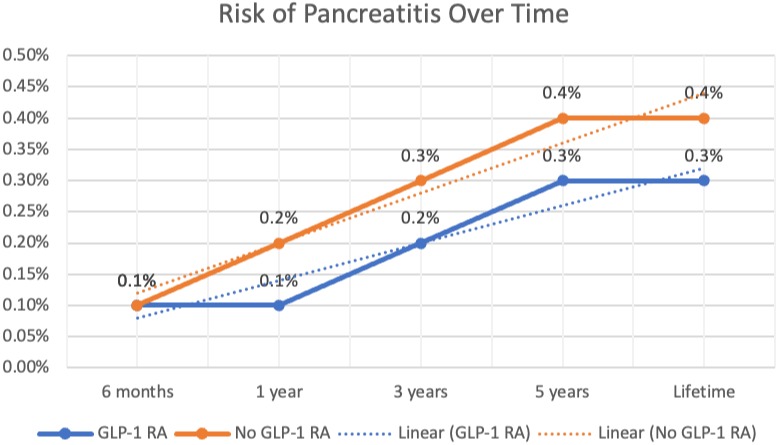
Figure: Linear graph of outcomes
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mark Ayoub indicated no relevant financial relationships.
Carol Faris indicated no relevant financial relationships.
Harleen Chela indicated no relevant financial relationships.
Veysel Tahan indicated no relevant financial relationships.
Roberta Hunter indicated no relevant financial relationships.
Ebubekir Daglilar indicated no relevant financial relationships.
Mark Ayoub, MD1, Carol Faris, MD2, Harleen Chela, MD1, Veysel Tahan, MD1, Roberta Hunter, MD1, Ebubekir Daglilar, MD1. P3494 - GLP-1 RA Does Not Increase the Risk of Pancreatitis in Patients with Type 2 Diabetes Mellitus: A U.S. Based Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
