Tuesday Poster Session
Category: Biliary/Pancreas
P3523 - GLP-1 Agonist Therapy: Culprit or Coincidence in Acute Pancreatitis? A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mohamed A. Ebrahim, MD
Ascension Saint Joseph Hospital
Chicago, IL
Presenting Author(s)
Award: Presidential Poster Award
Mohamed A. Ebrahim, MD, Sneha Dhakal, MD, Eli A.. Zaher, MD, Parth Patel, MD, Muhammad Sohaib Alvi, MD
Ascension Saint Joseph Hospital, Chicago, IL
Introduction: Acute pancreatitis (AP) presents a significant health burden with mortality rates ranging from 1% to 5%, primarily attributed to causes like gallstones, alcohol consumption, and hypertriglyceridemia. This condition, characterized by abdominal pain, nausea, and vomiting, can also result from less common triggers such as medication-induced factors, trauma, and anatomical anomalies. Subcutaneous semaglutide, a GLP-1 receptor agonist increasingly used for managing type 2 diabetes mellitus (T2DM) and weight control, has raised concerns regarding its potential association with pancreatitis.
Case Description/Methods: We present a 53-year-old female who visited the emergency room due to multiple episodes of vomiting over four days and sudden onset abdominal pain. She had started semaglutide treatment for weight loss five weeks earlier, with an initial dose of 0.25 mg weekly for two weeks, then incremental increase of dose to 0.5 mg weekly. Shortly after her fifth dose, she experienced vomiting and diffuse abdominal discomfort, followed by sharp epigastric pain. Computed tomography (CT) imaging of the abdomen revealed findings consistent with acute interstitial pancreatitis. The patient reported a recent weight loss of 5 pounds after starting semaglutide. Although she lacked typical risk factors, her symptoms began following an increased dose of the GLP-1 agonist, suggesting a possible connection to the acute pancreatitis.
Discussion: Clinicians should remain cautious for potential drug-induced acute pancreatitis (AP) in patients recently initiated on subcutaneous semaglutide, a GLP-1 receptor agonist, who present with AP symptoms. In such circumstances, it is strongly advised to promptly stop the use of subcutaneous semaglutide and begin appropriate treatments for acute pancreatitis, adjusting interventions according to the severity of the condition. Additionally, careful prescription of GLP-1 receptor agonists is advised for diabetic individuals with heightened susceptibility to AP. Despite this caution, GLP-1 receptor agonists are not absolutely contraindicated in patients with diabetes and a history of pancreatitis. Instead, healthcare providers may consider such therapy if the pancreatitis stemmed from a known cause that has been effectively managed. It is essential for providers to thoroughly discuss the risks and benefits of GLP-1 receptor agonist therapy with patients who have a history of pancreatitis and to remain vigilant for any signs of pancreatitis recurrence during treatment.

Disclosures:
Mohamed A. Ebrahim, MD, Sneha Dhakal, MD, Eli A.. Zaher, MD, Parth Patel, MD, Muhammad Sohaib Alvi, MD. P3523 - GLP-1 Agonist Therapy: Culprit or Coincidence in Acute Pancreatitis? A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mohamed A. Ebrahim, MD, Sneha Dhakal, MD, Eli A.. Zaher, MD, Parth Patel, MD, Muhammad Sohaib Alvi, MD
Ascension Saint Joseph Hospital, Chicago, IL
Introduction: Acute pancreatitis (AP) presents a significant health burden with mortality rates ranging from 1% to 5%, primarily attributed to causes like gallstones, alcohol consumption, and hypertriglyceridemia. This condition, characterized by abdominal pain, nausea, and vomiting, can also result from less common triggers such as medication-induced factors, trauma, and anatomical anomalies. Subcutaneous semaglutide, a GLP-1 receptor agonist increasingly used for managing type 2 diabetes mellitus (T2DM) and weight control, has raised concerns regarding its potential association with pancreatitis.
Case Description/Methods: We present a 53-year-old female who visited the emergency room due to multiple episodes of vomiting over four days and sudden onset abdominal pain. She had started semaglutide treatment for weight loss five weeks earlier, with an initial dose of 0.25 mg weekly for two weeks, then incremental increase of dose to 0.5 mg weekly. Shortly after her fifth dose, she experienced vomiting and diffuse abdominal discomfort, followed by sharp epigastric pain. Computed tomography (CT) imaging of the abdomen revealed findings consistent with acute interstitial pancreatitis. The patient reported a recent weight loss of 5 pounds after starting semaglutide. Although she lacked typical risk factors, her symptoms began following an increased dose of the GLP-1 agonist, suggesting a possible connection to the acute pancreatitis.
Discussion: Clinicians should remain cautious for potential drug-induced acute pancreatitis (AP) in patients recently initiated on subcutaneous semaglutide, a GLP-1 receptor agonist, who present with AP symptoms. In such circumstances, it is strongly advised to promptly stop the use of subcutaneous semaglutide and begin appropriate treatments for acute pancreatitis, adjusting interventions according to the severity of the condition. Additionally, careful prescription of GLP-1 receptor agonists is advised for diabetic individuals with heightened susceptibility to AP. Despite this caution, GLP-1 receptor agonists are not absolutely contraindicated in patients with diabetes and a history of pancreatitis. Instead, healthcare providers may consider such therapy if the pancreatitis stemmed from a known cause that has been effectively managed. It is essential for providers to thoroughly discuss the risks and benefits of GLP-1 receptor agonist therapy with patients who have a history of pancreatitis and to remain vigilant for any signs of pancreatitis recurrence during treatment.

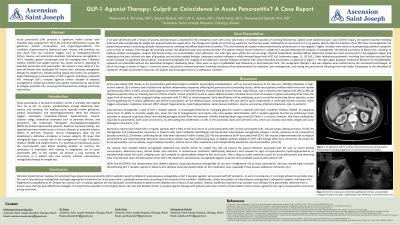
Figure: Figure 1. CT abdomen with IV contrast, denoting extensive peripancreatic inflammatory stranding suggestive of acute interstitial pancreatitis.
Figure 2. RUQ ultrasound, showing non-distended of gall bladder without any detectable echogenic shadow, no signs of gallbladder wall thickening or pericholecystic fluid.
Figure 2. RUQ ultrasound, showing non-distended of gall bladder without any detectable echogenic shadow, no signs of gallbladder wall thickening or pericholecystic fluid.
Disclosures:
Mohamed Ebrahim indicated no relevant financial relationships.
Sneha Dhakal indicated no relevant financial relationships.
Eli Zaher indicated no relevant financial relationships.
Parth Patel indicated no relevant financial relationships.
Muhammad Sohaib Alvi indicated no relevant financial relationships.
Mohamed A. Ebrahim, MD, Sneha Dhakal, MD, Eli A.. Zaher, MD, Parth Patel, MD, Muhammad Sohaib Alvi, MD. P3523 - GLP-1 Agonist Therapy: Culprit or Coincidence in Acute Pancreatitis? A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

